Osteoporosis - Diagnosis and Treatment
Overview
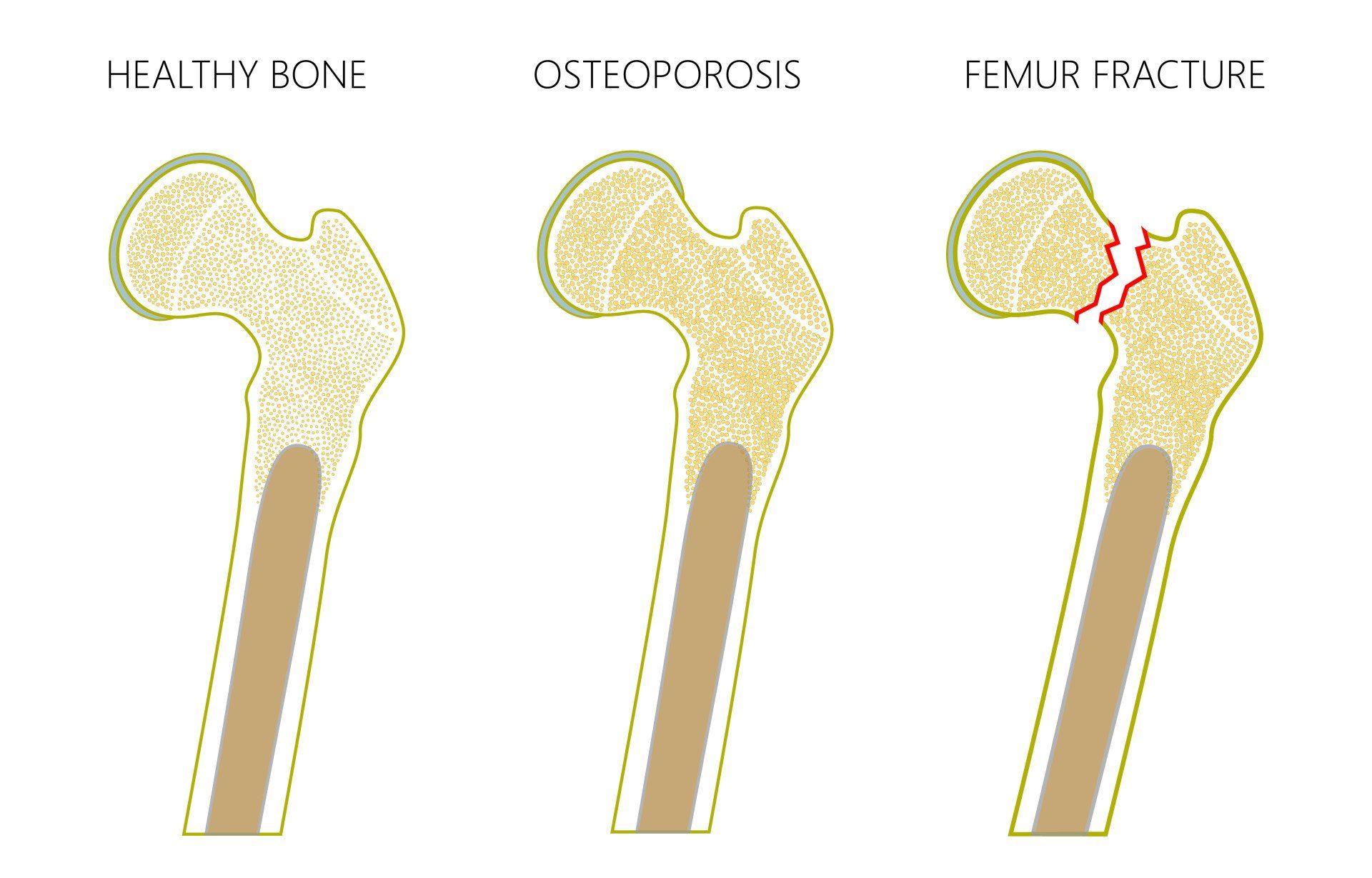
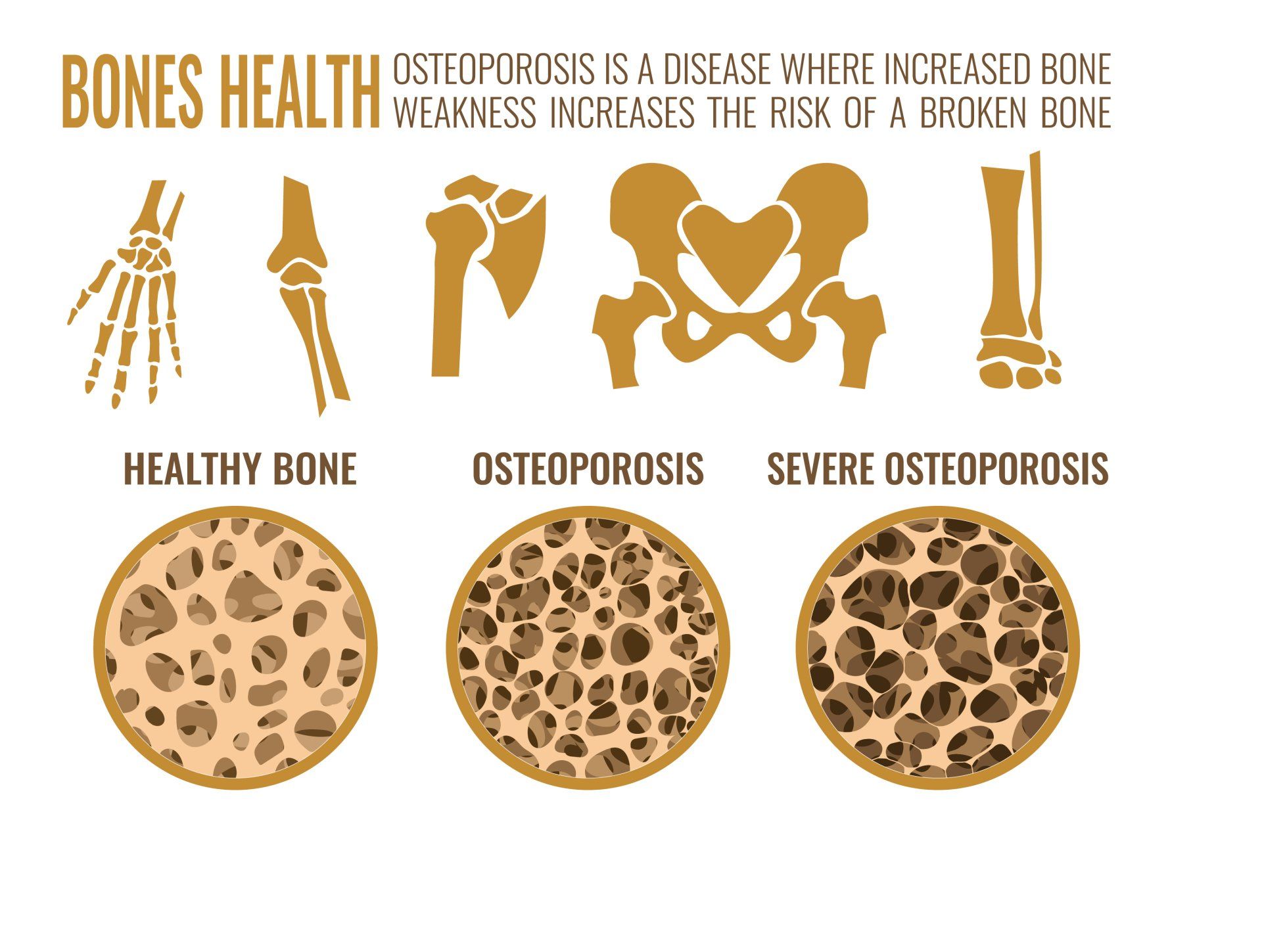
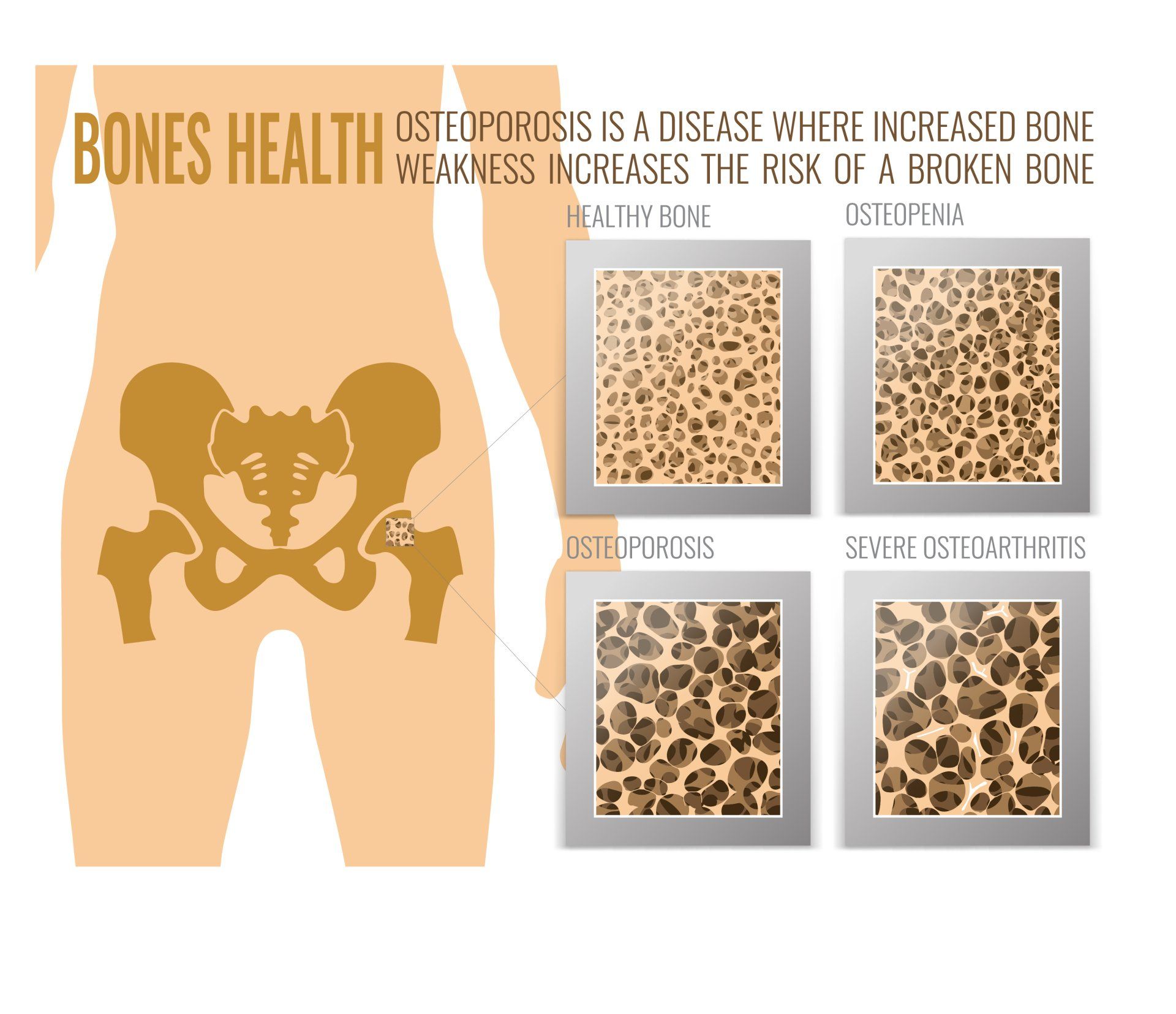
- Osteoporosis is significantly weakened bones that puts them at greater risk of fracture (breaking) from low energy trauma
- Osteopaenia is a milder version of osteoporosis
- Both are caused due to reduced bone density
- Osteoporosis is one of the commonest chronic diseases worldwide
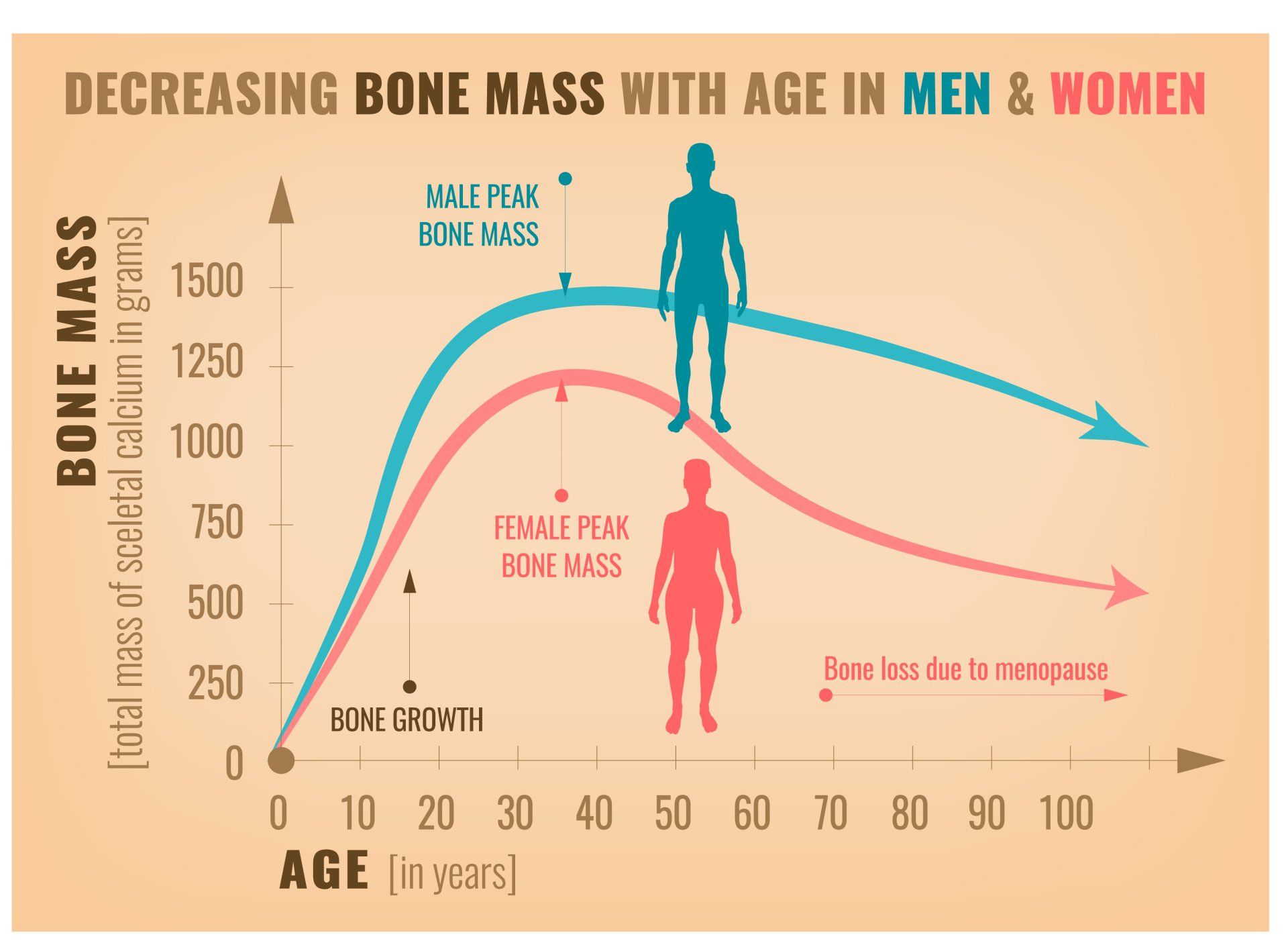
- Throughout life, new bone is formed (by cells in bone called osteoblasts) and old bone is removed through a process called resorption (by cells in bone called osteoclasts)
- The balance of this process is predominantly bone formation until peak bone mass is achieved after which it remains relatively stable until after menopause when the rate of bone loss predominates
- For more information on how to invest in your bones and minimise risk of osteoporosis later in life click here
- When this rate of bone loss is too great and depletes a critical level of bone material, it is termed osteoporosis
- Osteoporosis mainly affects women as their rate of bone resorption is greater than that of men especially in the early years following menopause
- Men can also get osteoporosis but are 4 times less likely
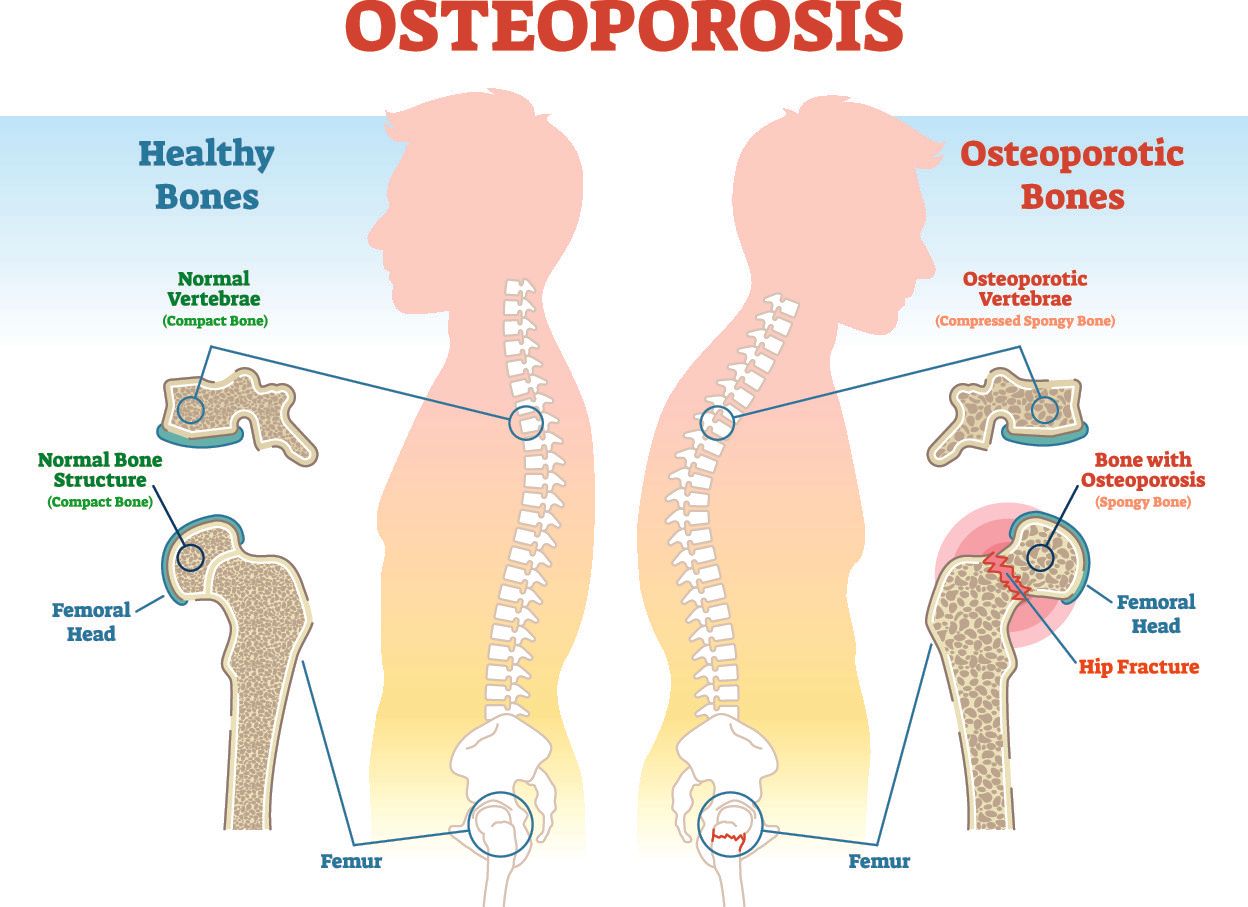
- Just 10% loss of bone mass in vertebrae will double the risk of fracture
- 10% loss of bone mass in hip will increase the risk of fracture by 2.5 times
- A prior osteoporotic fracture increases the risk of further fracture by 86%
- This means that more needs to be done to screen, diagnose and manage appropriately people over 50 years who have sustained a low energy fracture
How common is osteoporosis?
- Worldwide osteoporosis causes 9 million fractures every year:
- That’s one osteoporotic fracture every 3 seconds
- It is estimated to affect 200 million women worldwide:
- 10% of women in their 60s
- 20% of women in their 70s
- 40% of women in their 80s
- 66% of women in their 90s
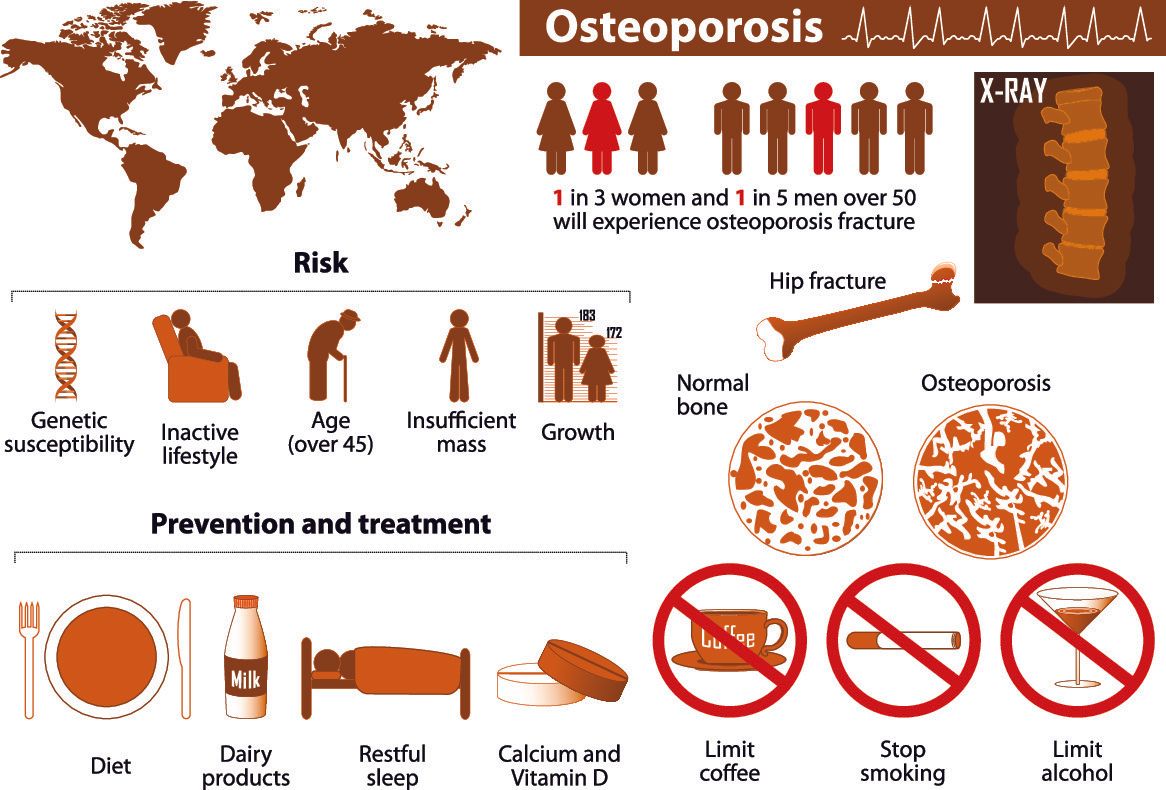
- 1 in 3 women and 1 in 5 men over 50 years will experience an osteoporotic fracture
- About 15% of Caucasians in their 50s and 70% of those over 80 have osteoporosis
- In the EU in 2010 ~22 million women and 5.5 million men had osteoporosis
- It affects ~80 million people in Europe, USA and Japan
- Due to the ageing population this will only increase:
- By 2050 incidence of hip fracture in men will increase by 310% and 240% in women compared to those in 1990
Osteoporosis in men
- Whilst women are 4 times as likely to get osteoporosis than men, men do still get it
- By ~70 years men and women lose bone mass at a similar rate
- Whilst men have lower risk than women of developing osteoporosis they have twice the mortality risk of women a year following their hip fracture
- There needs to be greater awareness in the public domain that men are not exempt from osteoporosis
Impact on disability
- Following an osteoporotic hip fracture:
- 40% cannot walk independently
- 80% cannot do basic activities of daily living independently such as shopping
- 10-20% of hip fractures require permanent care in a nursing home
- Osteoporosis in women over 45 years accounts for more days in hospital than heart attacks, breast cancer or diabetes
The financial burden of osteoporosis
- The financial impact of osteoporosis in the EU is €37 billion and in the USA $19 billion per year and is likely to double by 2050:
- 66% went to treatment of fractures
- 29% for long term care of fractures
- 5% for medications
- Therefore by improving osteoporosis prevention through nutrition, medication and exercise are very cost effective
- In 2010 in the EU the cost of long-term disability following osteoporotic fractures alone was almost €11billion
- Globally 40% of osteoporotic fractures occur in the working population:
- The annual cost of treating these fractures in Europe, USA and Canada is $48billion excluding the indirect cost of disability and loss of productivity
- The cost of osteoporosis treatment in Greece is estimated to be ~€900million
What is a fragility fracture?
- A fragility fracture is when a fracture (broken bone) results from low energy trauma such as a fall from standing height or less:
- Normally should be able to withstand such a fall without sustaining a fracture
- Osteoporosis is the major cause for this
- The most common location for fragility fractures are:
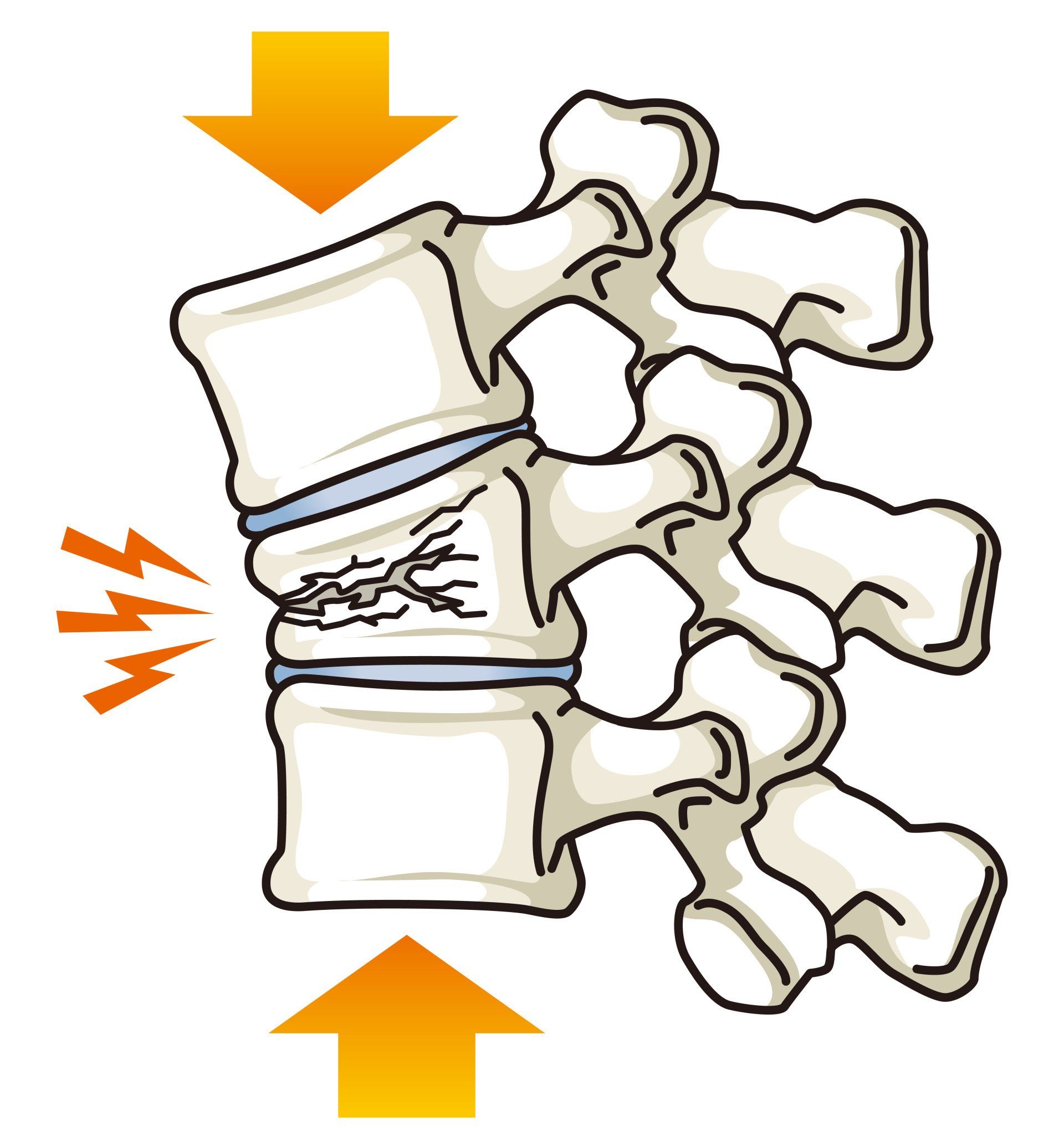
- Vertebral body (bone segment of the spine):
- They are the most common type of fragility fracture
- They often occur without a fall
- Hip:
- >85% of hip fractures are due to falls
- They carry the greatest mortality risk of the fragility fractures
- Typically occur in less mobile patients than wrist fractures as they have slower reflexes and don’t manage to break their fall using their hands
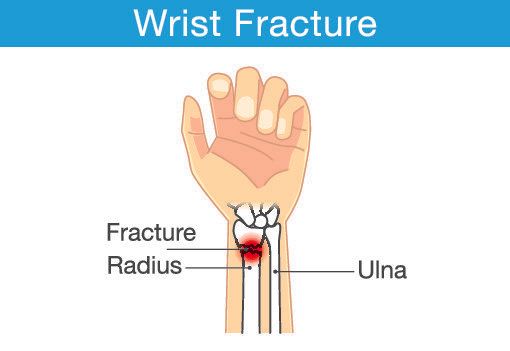
- Wrist:
- Is often the first indicator of osteoporosis if sustained after 50 years of age following low energy trauma
- The third commonest fragility fracture
- Tends to occur in more mobile and fitter patients with osteoporosis as they put their hand out to break a fall
- Half of all women and a quarter of all men will have a fragility fracture in their lifetime
- 80% of people who have had an osteoporotic fracture are neither identified nor treated
Hip fractures
- ~75% of all hip fractures occur in women and 25% in men
- Hip fractures are associated with chronic pain, reduced mobility, disability and loss of independence:
- 10-20% of independent patients require long term nursing care following an osteoporotic hip fracture
- The lifetime risk of hip fracture in white women is (1 in 6) more common than breast cancer is (1 in 9)
- Hip fractures by 2050 are predicted to triple
- Hip fractures have a mortality rate of ~10% at one month and 20-30% at 1 year post injury
- The higher risk of mortality persists for at least 5 years post injury
- There is marked loss of independence even a year later:
- 40% unable to walk independently
- 60% requiring assistance to walk
- 5-10% of patients with a hip fracture will experience another one within 3 years
Vertebral Fracture
- Vertebral fractures are the most common type of fragility fractures:
- One occurs every 20 seconds worldwide
- There is an 8 fold increase in mortality rate following one
- The lifetime risk of a vertebral fracture in a white 50 year old woman (16%) is three times greater than that of a 50 year old white man (5%)
- 30-45% of vertebral fractures go unnoticed i.e. patients don’t realise or don’t seek medical attention so many will be incidental findings at a routine check-up or visiting a doctor for something else
- Following a vertebral fracture there is an increased risk of another fracture elsewhere in the body in the next 1-2 years
- >55% of patients with a hip fracture show evidence of a previous vertebral fracture
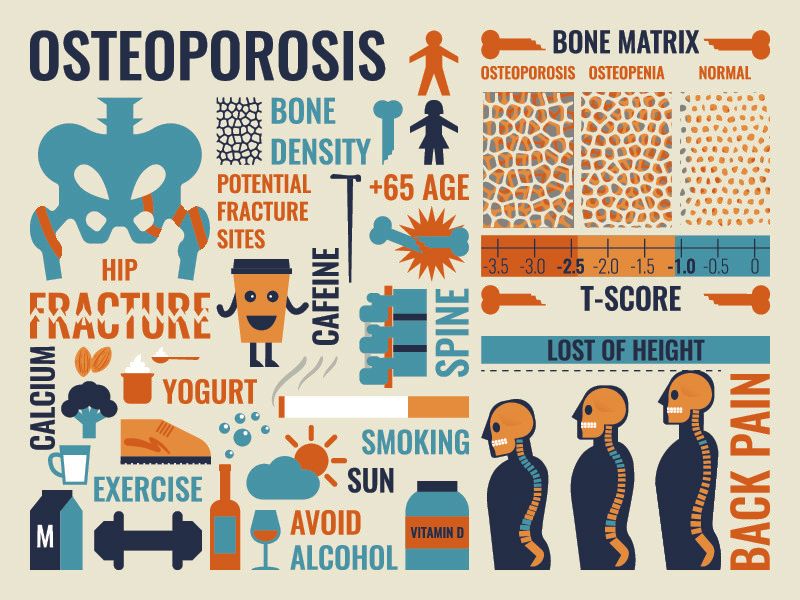
- Vertebral fractures can lead to:
- Back pain
- Loss of height
- Spine deformity (bent forwards)
- Reduced mobility
- Reduced lung function leading to greater shortness of breath and more susceptible to chest infections
- Reduced quality of life due to:
- Reduced mobility
- Reduced self-esteem
- Reduced body image
- Depression
- Difficulty carrying out activities of daily living i.e. ability to self-care:
- Feeding, cleaning, dressing, grooming
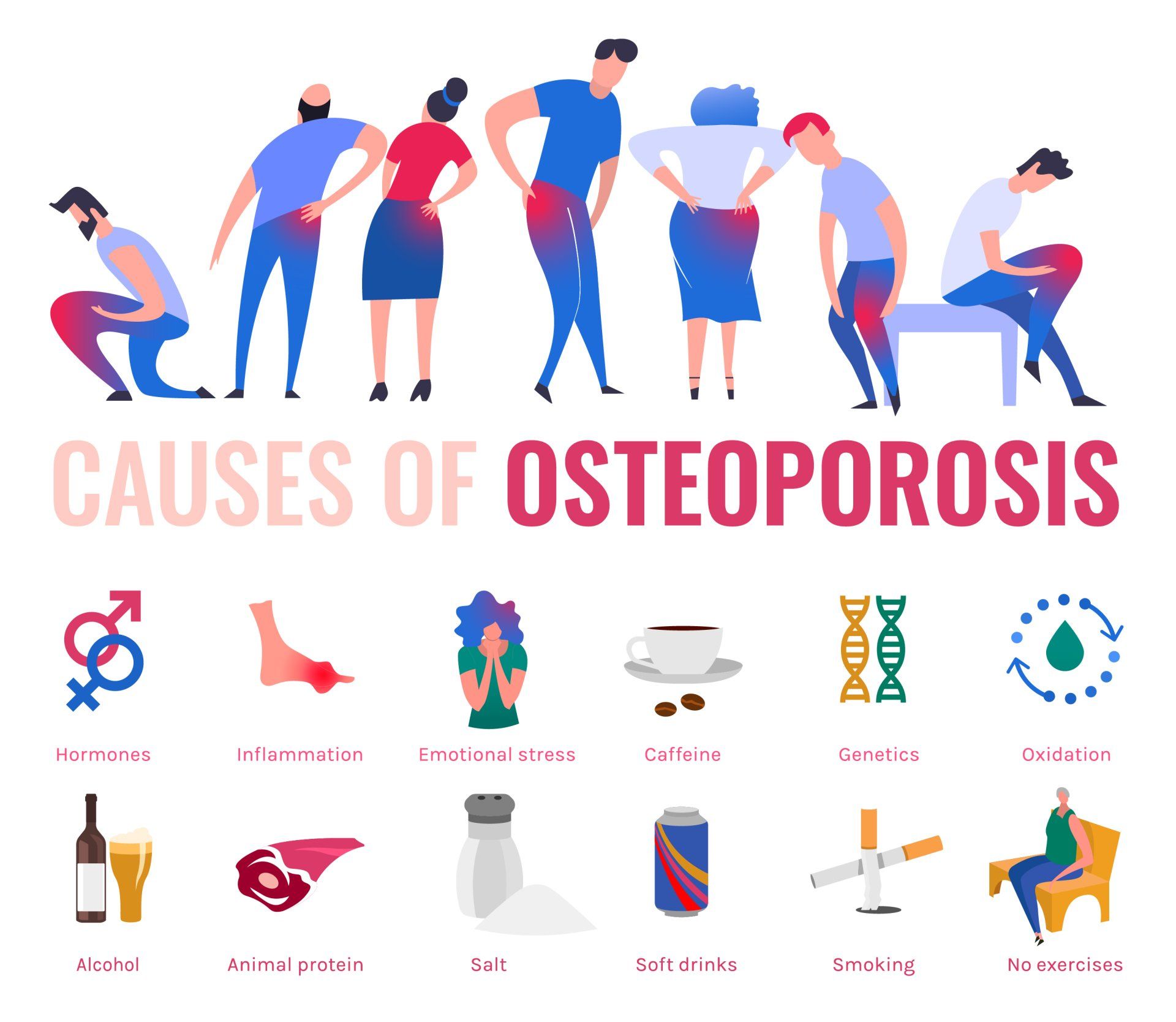
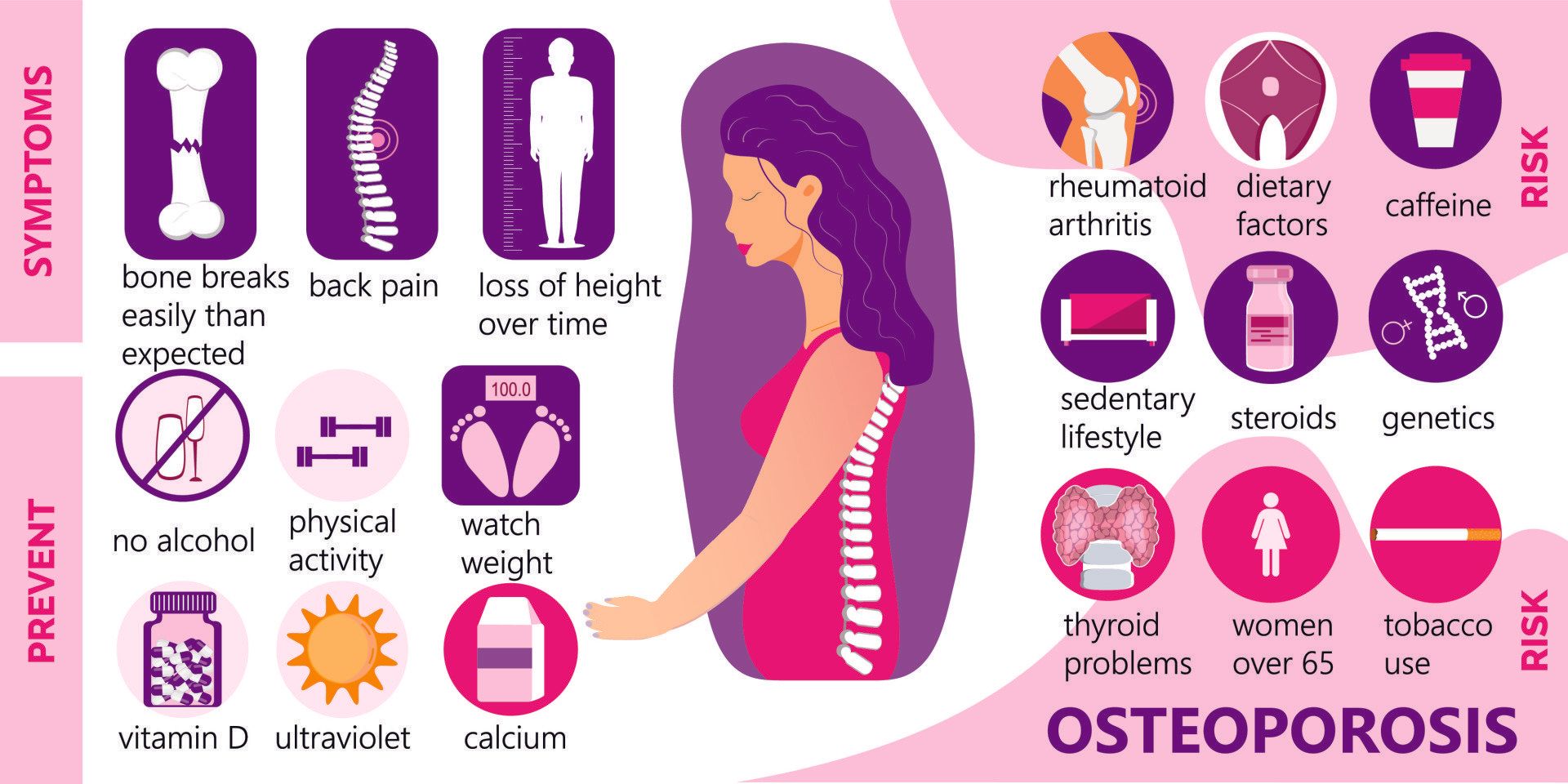
Risk factors for sustaining an osteoporotic fracture
- Although osteoporosis is defined in terms of bone mineral density, it is only one component of fracture risk, so the other risks need to be considered when assessing and managing someone’s osteoporosis and fracture risk:
- Genetic:
- Presence of hip fracture in parents is an independent risk factor to bone mineral density
- Lack of physical activity and living a sedentary lifestyle increase the risk of fragility fractures
- Low weight in infancy increases the likelihood of reduced bone mass in adulthood thus increasing risk of developing osteoporosis
- Smoking
- Alcohol
- Drinking >4 units a day doubles the risk of hip fracture
- Long term use of corticosteroids is the commonest cause of secondary osteoporosis:
- 30-50% of patients on long term corticosteroids risk of getting fracture
- Low body weight (BMI <20) is associated with increased risk of fracture
- Female Athlete Triad:
- Young females who train excessively, eat too little and have menstrual dysfunction are prone to low bone mineral density and increased risk of fractures
- Men and women >50 years who lose >0.5cm of height per year are at increased risk of fracture
- Long term intake (>2 years) of certain antacids called proton pump inhibitors (e.g. lansoprazole, omeprazole) reduce the absorption of calcium
- Falls are a major contributor to fractures:
- ~33% of people >65 years fall annually
- 90% of hip fractures are caused by falls
- 10-15% of falls in elderly will result in a fracture
- 60% of those who fall will fall again
- The risk of falls increases with age due to:
- Poor eyesight
- Poor balance
- Poor coordination
- Slower reflexes
- Reduced strength
- Increased risk of conditions that predispose to falls such as dementia, heart arrhythmias, fainting and seizures
Presentation
- Osteoporosis itself does not cause pain:
- There are no signs or symptoms until a fracture occurs
- Hence it is often termed a silent disease
- However, the broken bones that result cause pain and morbidity and can increase risk of mortality (especially hip fractures)
- When more severe, even a cough or a sneeze can cause a broken rib or collapse of bones (vertebrae) in the spine
- Elderly patients who have a stooped (bent forward) posture is often secondary to collapse of vertebrae in the spine
- Back pain in the elderly can be a sign of osteoporotic fracture in the spine
Osteopaenia
- Osteopaenia is a stage before osteoporosis:
- It has a higher bone mineral density than osteoporosis but is less than normal
- It does not always lead to osteoporosis but it is important to take measures to reduce risk of deteriorating to osteoporosis
How is osteoporosis and osteopaenia diagnosed?
- Osteoporosis cannot be diagnosed on plain X-rays:
- You can though get a feeling of reduced bone density without knowing the severity of it
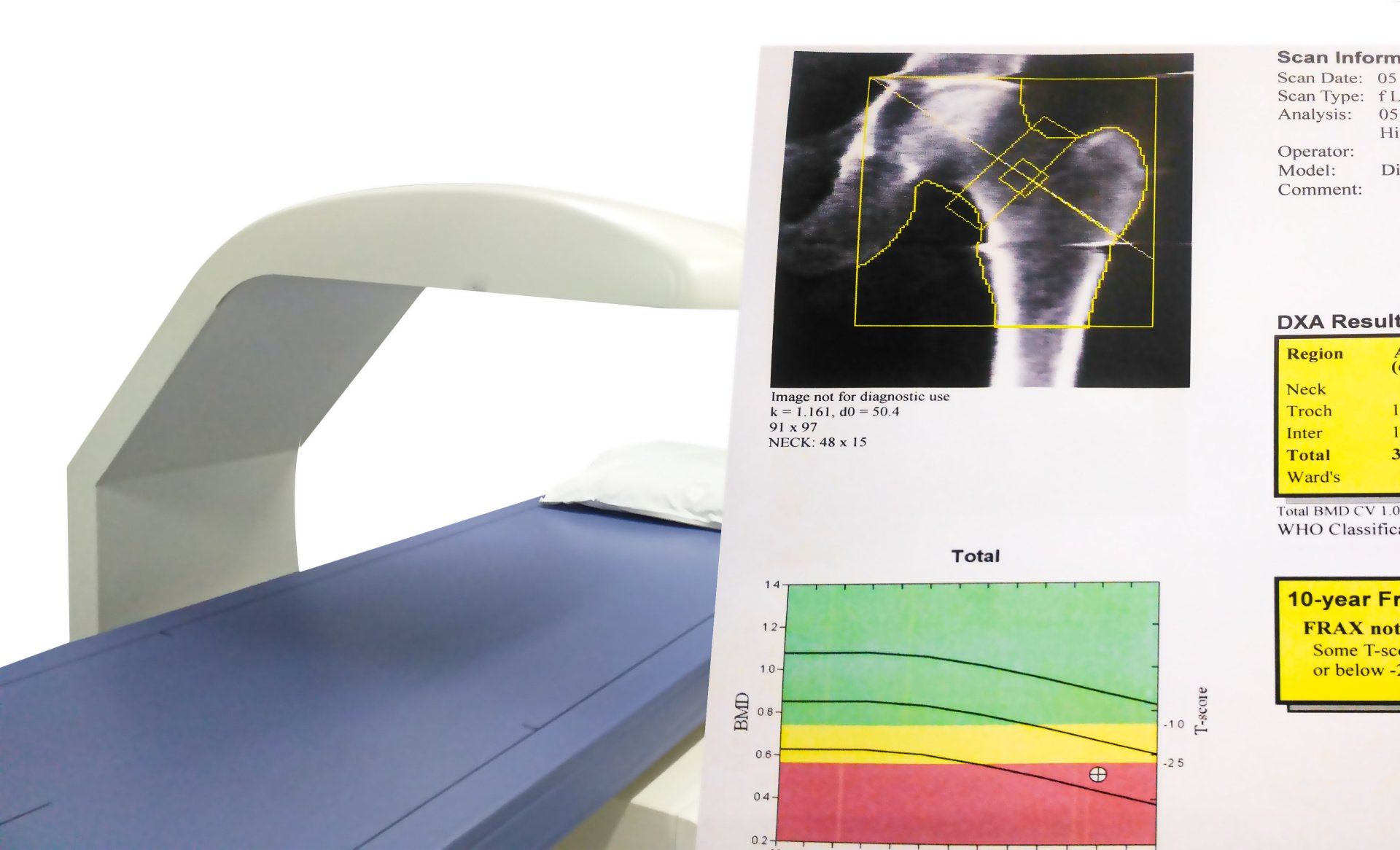
- The only way to diagnose osteoporosis and differentiate it from osteopaenia is through a DEXA scan:
- DEXA = Dual Energy X-ray Absorptiometry
- It is a non-invasive test
- Uses X-rays
- You lie on your back and it takes 10-20 minutes after which you can go home
- No injection is involved and you won’t go into a tunnel like some other scans
- Osteopaenia will show up on X-ray after 40% loss of bone density
- DEXA scan can detect changes as small as 1%:
- It is therefore more sensitive and accurate than plain X-rays
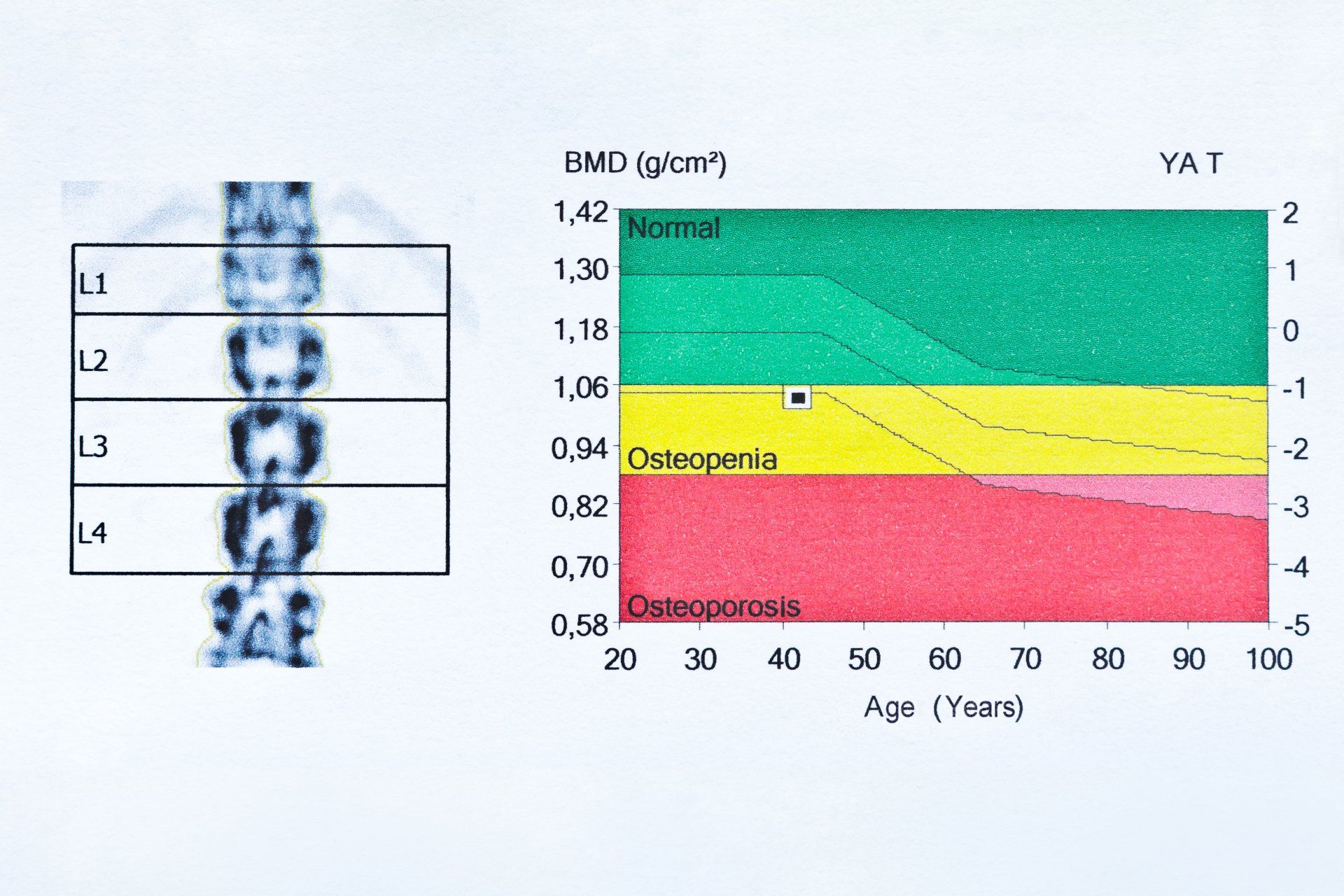
- DEXA scan results are reported using T-scores
- A T-score is a number that is relative to how much the measured bone mineral density differs from the mean mineral bone density of a healthy 30 year old person
- It is measured in standard deviations away from the mean
- Normal T-score as per the World Health Organisation (WHO) is within 1 standard deviation from the mean:
- That means anything greater than -1 is normal e.g. +0.5 or -0.9 (which is worse than +0.5)
- Osteopaenia is defined by a T-score that is between -1 to -2.5 i.e. between 1 and 2.5 standard deviations below the mean value e.g. -1.1 or -2.4 (which is worse than -1.1)
- Osteoporosis is defined by a T-score that is below -2.5 i.e. more than 2.5 standard deviations below the mean e.g. -2.6 or -3.5 (which is worse than -2.6)
- In the T-score graph below age is shown on the x-axis (horizontally), bone mineral density on the left y-axis (vertical axis) and T-score on the right y-axis:
- The top green zone is normal bone mineral density and represents values greater than -1.0
- The middle yellow area shows osteopaenia zone between -1.0 and -2.5
- The lower red area shows the osteoporosis zone which is anything below -2.5
- Z-score is another scale often used in relation to osteoporosis:
- Whilst it is not used to diagnose osteoporosis it can provide useful information especially when it is secondary to a coexisting illness and is found in the less common groups of people e.g. children, young adults, pre-menopausal women and men under 50 years of age
- It compares patient’s bone density to the mean bone density of someone of the same age, sex and ethnicity
- There are numerous tools used to assess an individual’s fracture risk at 10 years and this helps guide their management
Screening
- There are numerous screening tools that can help identify high risk patients that would benefit from formal screening of osteoporosis
- Current guidelines on screening recommend all women over 65 years and men over 70 years should be screened with a DEXA scan
- Anyone over 50 years who is high risk such as:
- Previous bone fracture from low energy trauma e.g. hip fracture
- Low body weight
- Excessive smoking or alcohol
- Patients who have an increased risk of osteoporosis should consider earlier screening
- All post-menopausal women who have incurred a fracture
- Any wrist fracture sustained following a minor fall in those over 50 years
Treatment
- Treatment is guided not only by the DEXA scan T-score but also by the risk factors each patient has for osteoporosis
- Recognition and treatment of a fragility fracture can help reduce the risk of future fractures by 50%:
- With the added benefit of preventing exposure to the additional morbidity and mortality risks that occur following a fragility fracture
- Effective medical treatment can reduce the risk of:
- Vertebral fracture by 50%
- Hip fracture by 40%
- Other fractures by 20%
- Poor compliance (patients not following doctor’s advice) is one of the most important issues at effectively combatting osteoporosis:
- Only 40% of patients continue to take their treatment after a year
- Only 20% of patients continue to take their treatment after two years
Exercise
- Exercises that help people with osteoporosis should focus on strengthening bones, muscles and preventing falls through the following types of exercises:
- Weight-bearing:
- Exercises that are minimal or non- weight bearing offer little benefit to improving bone strength
- Strengthening:
- Helps put load on bones that over time will make them denser and stronger
- Balance:
- This is key and often forgotten exercise that will help prevent falls
- Flexibility:
- Helps improve overall physical function
- Must avoid exercises that flex the spine such as sit ups in order to avoid fractures in the spine
- Posture:
- Focusing on strengthening spine extensor muscles
- Helps prevent kyphosis and risks of falls
- Exercise during childhood and adolescence is particularly important in order to gain bone mass
- Regular exercise helps reduce risk of:
- Osteoporosis
- Fracture
- Injuries due to falls
- Strengthening back muscles helps reduce risk of vertebral fractures and kyphosis (excessive forward curve of the spine)
- Activities that help improve balance and confidence in the elderly help prevent falls and subsequent injuries:
- Tai chi has been shown in some studies to help reduce falls by 50% and hip fractures by 25%:
- Tai chi is an ancient Chinee martial arts that focuses on slow movements and deep breaths
- Helps to reduce stress, anxiety, depression
- Improves muscle strength, balance, flexibility, stamina
- Minimal impact on joints so safe to do in presence of arthritis
- Yoga:
- Can also be beneficial for the elderly with osteopaenia and osteoporosis
- However, patients should avoid positions that involve:
- Spinal flexion (forward bending of back)
- Extreme twists and sidebends
- They can increase the risk of an inadvertent fracture in the spine
Nutrition
- Children during their growth should have adequate intake of calcium in order to maximise the beneficial effect of exercise in boosting bone mass which will be beneficial for them during their elderly years
- Postmenopausal women who take calcium tablets improve their bone mineral density
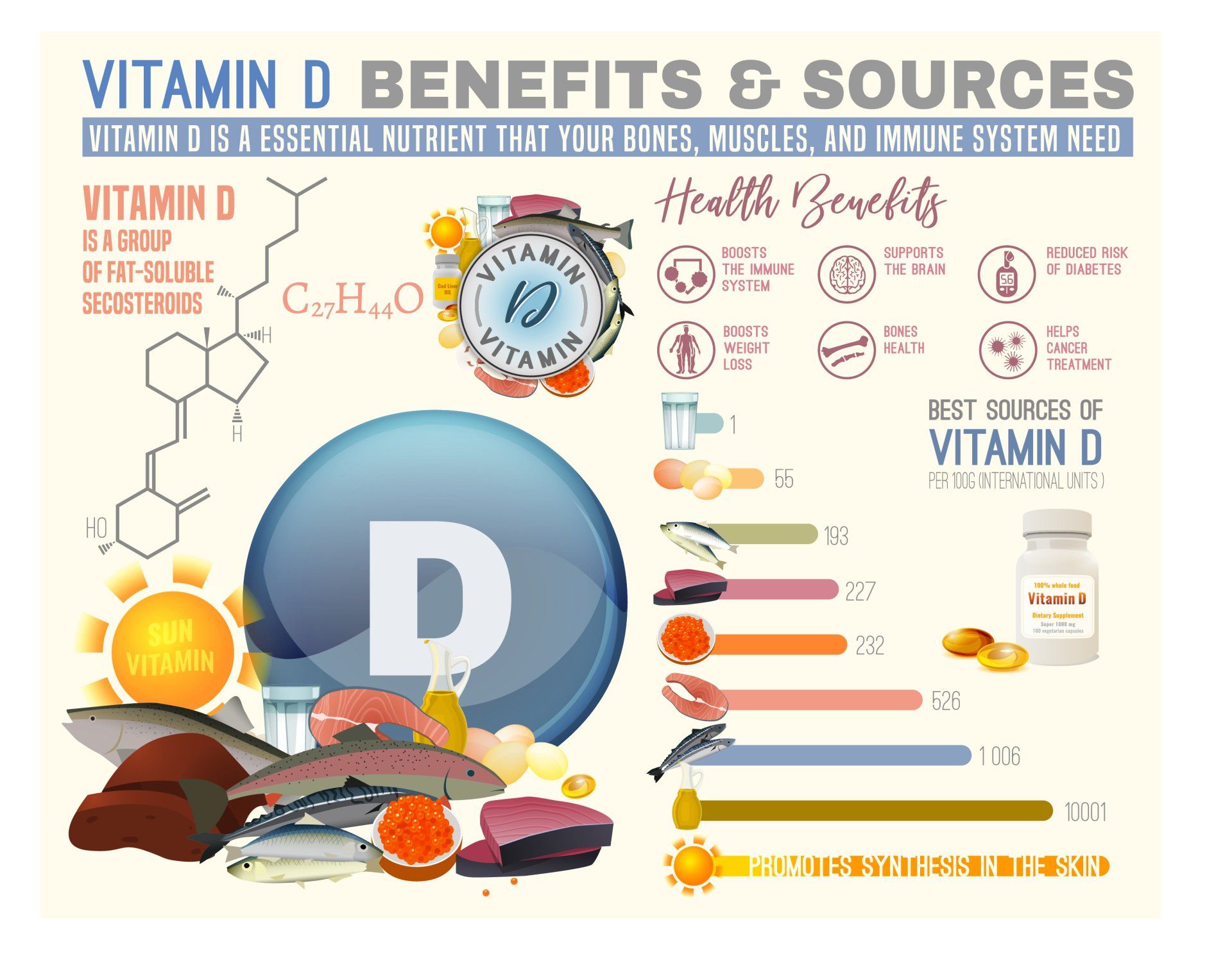
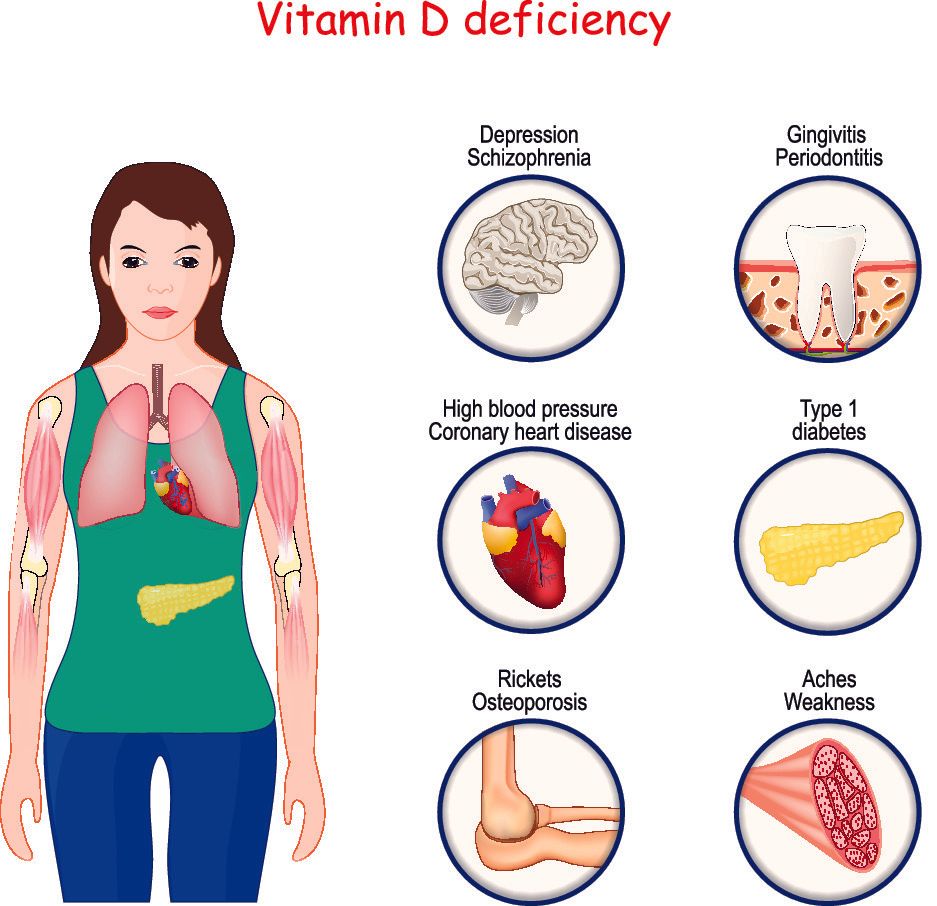
- One of the key risk factors in osteoporosis and route for prevention and treatment of osteoporosis is vitamin D
- The elderly are particularly prone to low vitamin D levels as they are often indoors and receive suboptimal sun exposure
- Fruit, vegetables and good protein intake have been shown to lower rate of bone loss with age
- Good nutrition is essential for those who have sustained a hip fracture especially the more frail and elderly patients:
- Failure to address this slows recovery and increases risk to further fracture
- Those with lactose intolerance and those who drink less milk have increased risk of lower bone mass
- Whilst mild to moderate alcohol intake is not harmful, chronic alcohol abuse (>4 units daily) greatly reduces bone mineral density
- Anorexia nervosa is an eating disorder and mental health illness characterised by persistent restriction of calories consumed, abnormally low weight, intense fear of gaining weight, and disturbed self-perceived weight or shape:
- Its onset is typically during puberty which is the period of gaining maximal bone mass and thus putting patients at high risk of reduced peak bone mass and subsequent early osteoporosis
Falls Prevention
- Whilst treatment of osteoporosis and making the bones stronger is beneficial and helps prevent bone fractures, taking measures to minimise the risk of falls is even more important
- Falls prevention can be simple to carry out and effective but not very well carried out and often forgotten
- Try and let someone know where you are and keep regular contact with people
- Carry a portable phone at all times in order to be able to call for an emergency
- If living alone, consider using a monitoring company that can be accessed 24/7
- Outdoors:
- Wear rubber soled shoes to improve traction and avoid high heels
- Taking care in the winter especially when there is rain, frost or snow:
- If unsteady on feet and need to go out try holding on to someone with better balance
- Leaves on the ground can be particularly slippery especially when wet
- Keep the walkways and driveways around your house free of rubbish, and tidy so as to prevent tripping over things
- Have good lighting outside your house when it goes dark
- Use a walking aid that has good rubber grip to the ground
- Taking care when walking on smooth polished surfaces e.g. marble especially if they are wet as they can be very slippery
- Being observant of the ground surface when walking outside:
- Uneven ground e.g. from pavement slabs, cobblestones
- Pot holes
- When stepping on and off from pavements and road curbs
- Indoors:
- Floors:
- Ensure any carpets are secured down well especially the edges
- Keep floors tidy free of clutter
- Wires and cables should be secured around the edges of walls and not go across pathways
- Bathroom:
- Use a non-skid rubber mat in shower/bath as well as outside of it where you step off
- If unsteady on feet, consider placing a plastic chair with back and rubber covered feet to minimise skidding
- Consider walk-in and zero-entry showers that have no step and so helps prevents falls whilst transferring in and out of showers
- Install rails around bath, shower and toilet
- Try and keep the walkway between bedroom and bathroom tidy
- If tend to go to toilet in middle of the night consider leaving light on in walkway
- Bedroom:
- Ensure there are light switches by the door and around bed and bathroom
- Whenever getting out of bed, take your time, sit on edge of bed and wait until more alert before getting out of bed in order to prevent dizziness and fainting:
- Common cause of hip fractures in the elderly is falling between bedroom and bathroom in middle of the night
- Have a flashlight handy on bed side table
- Stairs:
- Sturdy hand rails on both sides
- Keep the area well lit, with light switches top and bottom and free of any objects
- If there are carpets ensure they are secured well and if hard surface that they are clean and dry
- Kitchen:
- Use non-skid mats around the sink and hob
- Any spills should be cleaned up immediately
Reducing the impact of a fall
- Try if possible to fall forward or on buttocks and to break the fall using your hands:
- This helps reduce chance of a hip fracture which is a bigger health risk than a broken wrist
- Walk carefully on hard surfaces
- Do not run on hard surfaces:
- If the phone rings do not rush to get it
- Wear protecting clothing
Medication for osteoporosis
- The purpose of the medication is to increase bone density
- Over the first 3 years of treatment bone density in the hip can increase by 1-3% and in the spine by 4-8%
- Medication can help reduce the risk of hip fracture by 30-50% and in the spine by 50-70%
- However, these benefits are not instant and they start to be seen 6-12 months after commencement of medication
- Generally speaking osteopaenia requires monitoring, improvement in nutrition and exercise, and consideration of calcium and vitamin D supplements
- For confirmed osteoporosis or those with osteopaenia but a high 10 year fracture risk, additional medication should be considered
- There are numerous types available which are often in addition to calcium and vitamin D medications
- The first line are usually bisphosphonates and they are the most commonly used medication:
- E.g. Alendronate (Fosamax), Risedronate (Actonel), Zolendronate (Reclast)
- They work by inhibiting the actions of bones cells called osteoclasts that resorb bone
- They can reduce the risk of fracture by 25-70%
- They are not absorbed will in the stomach and can cause stomach upset and heartburn
- Recommendation is to take them on an empty stomach with plenty of water and to remain sitting up for at least 30-60 minutes and then to have breakfast:
- Bending over or lying down will aggravate the heartburn
- They take 6-12 months to take effect on the bones
- There is little evidence that they add benefit for most patients after 3-5 years of use after which time rare potential side effects arise:
- Atypical femoral fractures as the bones get too strong and brittle
- Osteonecrosis of the jaw - the jaw bone can start to die off
- For high risk patients can consider taking them for 10 years
- Other commonly used medications include:
- Denosumab (Prolia):
- Newer medication that is better tolerated than bisphosphonates
- Is a monoclonal antibody and works by preventing development, function and survival of bone resorbing cells called osteoclasts
- Taken as an injection twice a year
- Should not be taken if blood calcium is low
- Like bisphosphonates can rarely cause atypical femoral fractures and osteonecrosis of the jaw after prolonged use
- Teriparatide (Forteo):
- Is a form of parathyroid hormone and stimulates bone forming cells called osteoblasts to lay down new bone
- Side effects include leg cramps, nausea and dizziness
Further helpful information can be found here on:

Introduction Cubital Tunnel Syndrome occurs when the ulnar nerve is compressed within a tunnel on the inner (medial) side of the elbow just behind the bony prominence of the inner aspect of the elbow called the medial epicondyle Cubital Tunnel Syndrome is the second most common cause of peripheral nerve compression: The most common one being carpal tunnel syndrome (compression of the median nerve at the wrist) The ulnar nerve is one of the three main nerves of the upper limb: The other two nerves of the upper limb are the median nerve and the radial nerve The ulnar nerve travels from the neck past the elbow and wrist and into the hand: Along the way it travels past some narrow areas where it can be constricted and cause symptoms for the patient The most common site of ulnar nerve compression is in the cubital tunnel at the elbow The second most common site is in Guyon’s canal in the hand When someone accidentally hits the inner side of the elbow (often termed hitting the funny bone) they get a sharp tingling sensation on the inner side of the elbow and forearm: This occurs because the ulnar nerve was hit at the site of the cubital tunnel where the nerve is close to the skin surface and therefore easily injured from outside forces
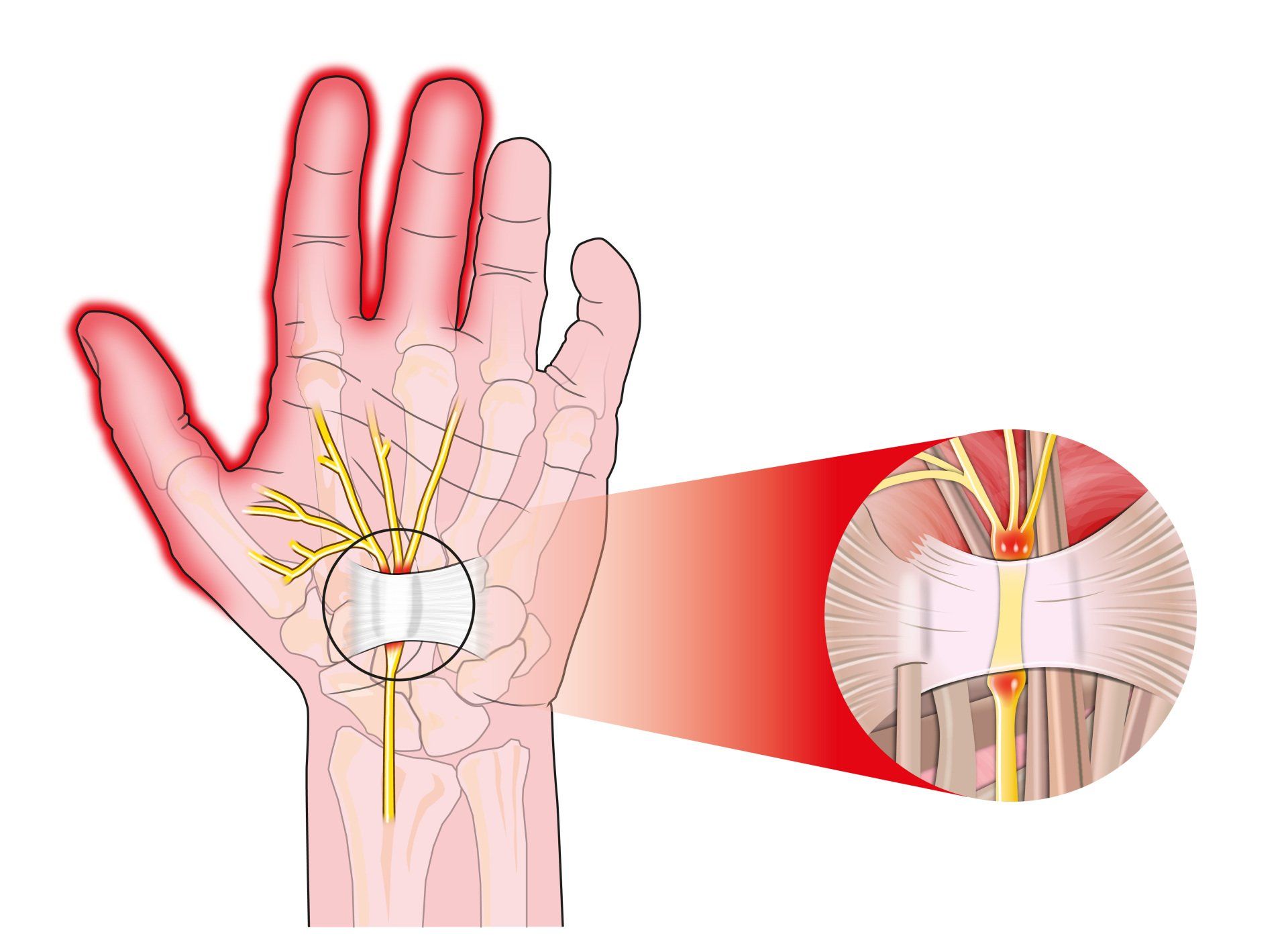
Introduction Carpal tunnel syndrome is a common condition that causes numbness, tingling and weakness in the hand specifically affecting the thumb, index and middle fingers: The little and ring fingers are not affected as they are supplied by another nerve called the ulnar nerve It is the commonest cause of peripheral nerve entrapment It is caused by compression of the median nerve as it passes from the forearm into the hand through a passage called carpal (i.e. wrist) tunnel The median nerve is one of three main nerves that supply the upper limb: The other two nerves are the ulnar nerve and the radial nerve
Introduction Tennis elbow (also known as lateral epicondylitis) is an overuse injury of the forearm tendons that originate over the lateral epicondyle of the humerus (bony prominence on the outside of the elbow) and act to bring the wrist backward away from the palm Whilst tennis players are particular prone to this condition it does not occur exclusively to them

Introduction This term is also known as repetitive motion or stress injury and occurs as a result of carrying out the same motion repeatedly over time causing injury to muscles and tendons It is associated with repetitive tasks, sustained or awkward position, forceful exertion, vibration or compressive forces It can affect almost any joint in the body Most commonly affected areas are hands, wrists, shoulders and neck It is thought to affect 5-10% of the general population but can be as high as 20-40% in specific working populations