Vitamin D – The Unappreciated Vitamin
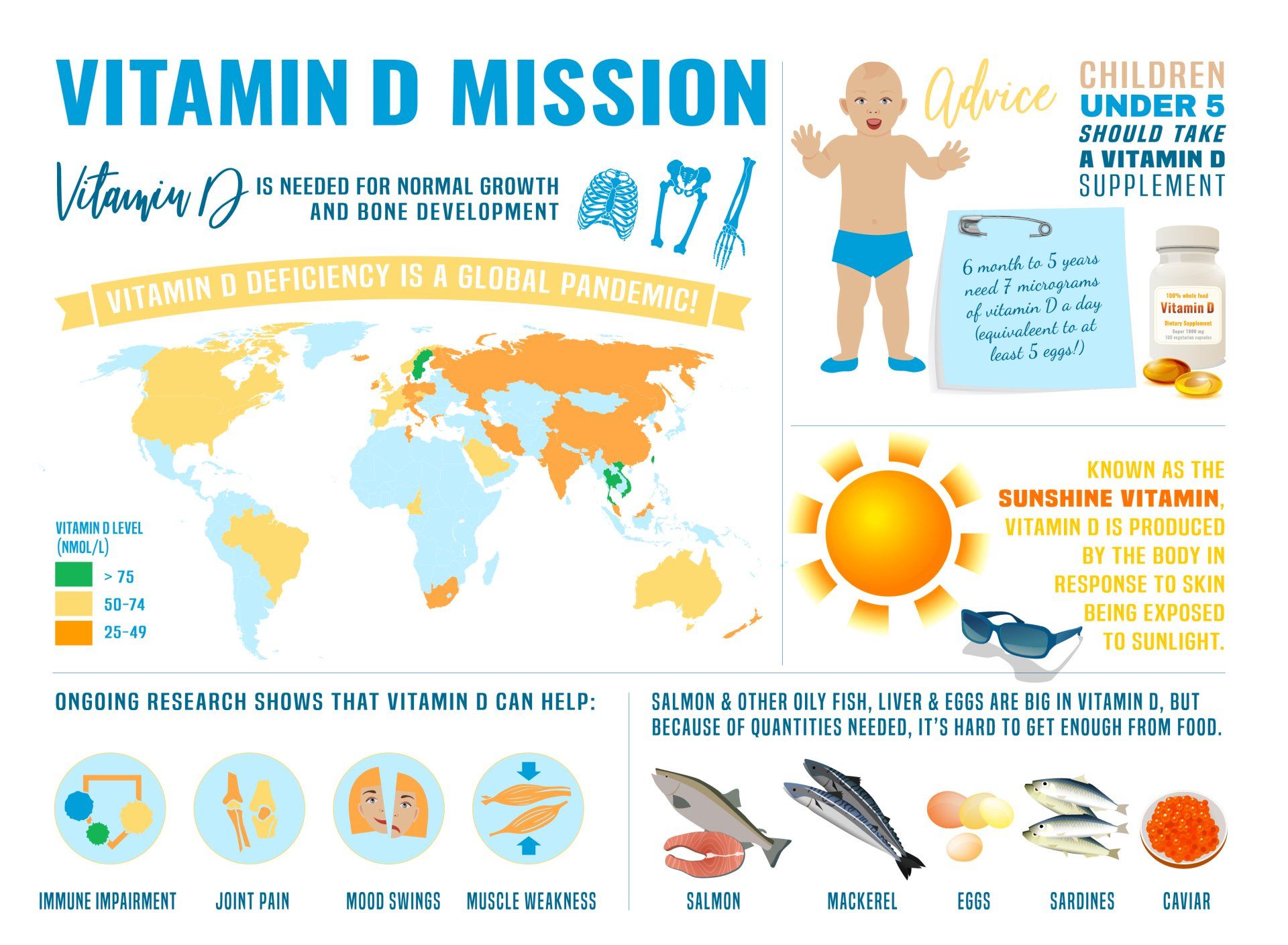
Vitamin D deficiency continues to be a global pandemic
- Vitamin D Deficiency is a recognised pandemic:
- It not only affects countries with low amounts of sunshine but also those that have lots of it
- Vitamin D deficiency is thought to affect over 1 billion people worldwide
- Over 77% of people in USA are considered to have vitamin D deficiency and this has become worse over the last 30 years
- Vitamin D has the unique property than unlike any other vitamin it can be produced by the body (from sunlight) and is not entirely reliant on diet consumption:
- Hence it’s often called the sunshine vitamin
- It is a fat soluble vitamin that is found naturally in very few foods
- The biggest and easiest contribution of vitamin D in body is through ultraviolet rays (UVR) from sunlight exposure which stimulates the body to produce its own vitamin D
- Other sources of Vitamin D are through:
- Medications
- Food fortified with vitamin D
What is the function of Vitamin D?
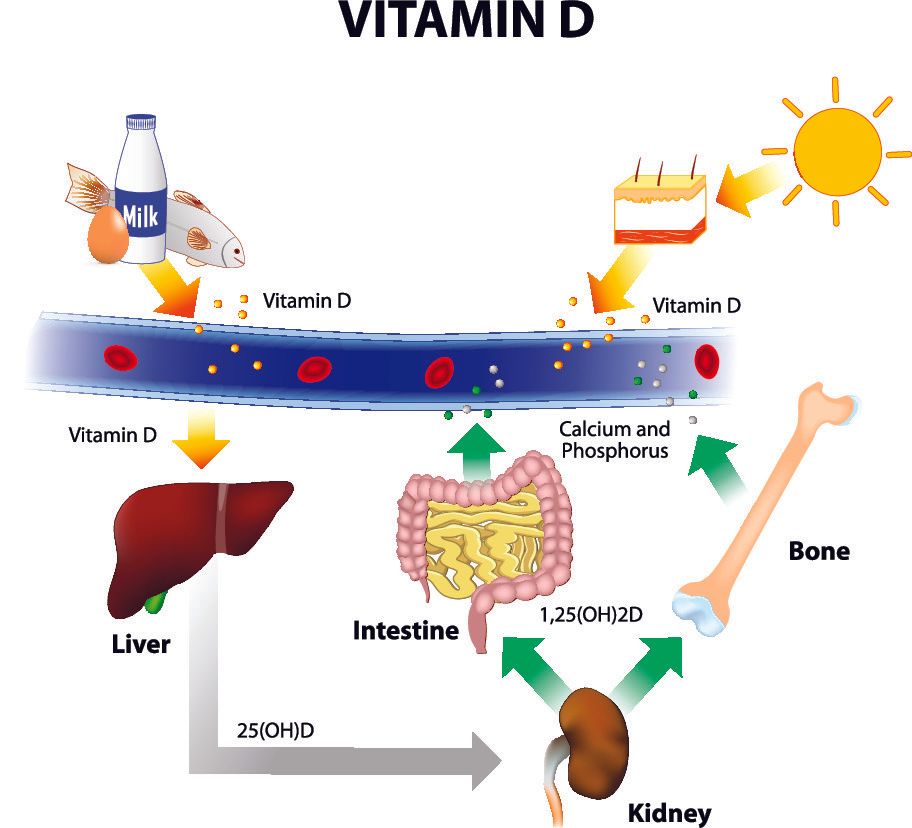
- Vitamin D increases calcium and phosphate absorption from the intestines
- Vitamin D inhibits the effect of parathyroid hormone on bones:
- Parathyroid hormone stimulates cells in the bone called osteoclasts to remove bone in a process called resorption
- Vitamin D insufficiency (and to a greater extent deficiency) is unable to inhibit this process so with more bone resorption come reduced bone density and osteoporosis
- Vitamin D receptors have been found in almost every tissue in the body meaning that it has an effect throughout the body
- >80% of the body’s vitamin D is involved in essential body functions such as:
- Synthesis of proteins and hormones
- Immune and inflammatory responses
- Cell turnover and synthesis
- Regulation of gene expression:
- Gene expression is the process by which a gene produces the functional product that it codes for
- This essentially means that without vitamin D the cell is unable to adequately respond to normal physiological signals as well as pathological ones
How is vitamin D synthesised from sunlight?
- During sun exposure UVB rays penetrate the skin and is absorbed by a cholesterol (7-dehydrocholesterol)
- Vitamin D exists in two forms:
- Vitamin D3 is produced in the skin from sun exposure
- Vitamin D2 is produced by plants
- Both types are found in supplements
- But D3 is more beneficial than D2 which is only 20-40% as effective as D3
- Both vitamin D3 and D2 are prehormones and need to be hydroxylated in two steps to become active:
- First in the liver to form 25-hydroxyvitamin D (also called calcidiol)
- It then travels in the blood stream to the kidneys where the second round occurs forming 1,25-hydroxyvitamin D (also called calcitriol) which is the only active form of the vitamin
- This last step is regulated by blood levels of calcium, phosphorus, and parathyroid hormone
Vitamin D deficiency vs insufficiency
- Numerous authorities have different levels on what constitutes deficiency and insufficiency
- The level of 25-hydroxyvitamin D in the blood stream is the best assessment of vitamin D in the body
- The American Endocrine Society defines them as:
- Deficiency: 50nmol/l (<20ng/ml)
- Insufficiency: 50-75nmol/l (20-30ng/ml)
- As per the American Endocrine Society, for marked beneficial effects of Vitamin D the blood level of 25-hydroxyvitamin D should be >75nmol/l (30ng/ml):
- However, for optimal benefit the target should be 100nmol/l (40ng/ml)
How much vitamin D should I take?
- The body requires 3000-5000IU of vitamin D daily for normal healthy function
- The daily requirement of Vitamin D remains controversial because:
- The daily requirements and recommendations were designed more to prevent deficiency than to achieve a level that recent studies suggest are needed to achieve maximal benefits from vitamin D
- Vitamin D is also synthesised from sunlight so dietary requirement and supplementation will also depend on effective exposure to UVB rays and degree of skin pigmentation
- People absorb dietary vitamin D quite variably
- Over time research has shown that we should be taking greater amounts than what we previously thought
- Oral vitamin D supplementation therefore should be guided by the level of 25-hydroxyvitamin D in the bloodstream:
- The ideal target concentration is 75-100nmol/l
- As per the American Endocrine Society, for marked beneficial effects of Vitamin D the blood level of 25-hydroxyvitamin D should be >75nmol/l (30ng/ml):
- However, for optimal benefit the target should be 100nmol/l (40ng/ml)
- Initial vitamin D dosage will depend on how severe the deficiency is
- Dosage up to 10,000IU per day have been found to be safe when the deficiency is severe or there is resistance to improving the vitamin D levels
- If there is inadequate sun exposure 800-1000IU of vitamin D3 is recommended and the level titrated pending on the patient’s response:
- Some people absorb vitamin D better than others so they may need even higher concentration of vitamin D3 in their medication in order to achieve the recommended level in the blood stream
| Age | Recommended intake (IU/day) | Upper limit (IU/day) |
|---|---|---|
| 0-12 months | 400 - 1000 | 2000 |
| 1-18 years | 600 - 1000 | 4000 |
| 19-70 years | 600 - 2000 | 10,000 |
| >70 years | 800 – 2000 | 10,000 |
| Pregnancy/Lactation | 600 – 1000 (14-18y) | 10,000 |
| 1500 – 2000 (19-50y) |
IU: International Units
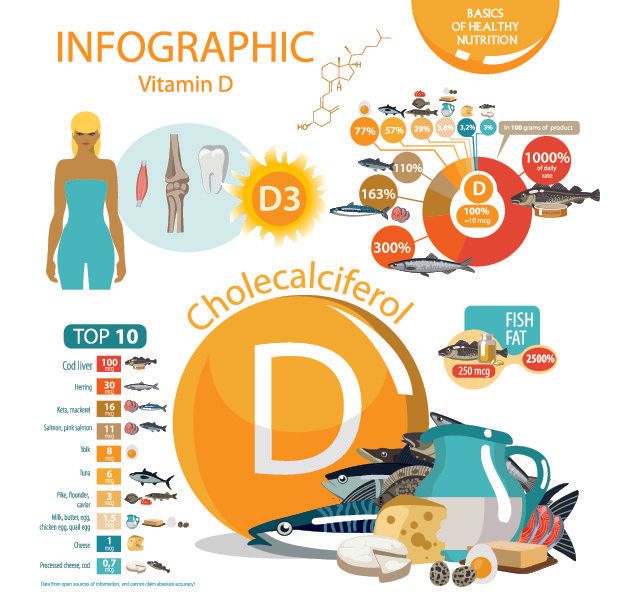
Which foods are high in vitamin D?
- Very few foods naturally contain vitamin D
- Foods that have significant amount of vitamin D are:
- Oily fish like tuna, mackerel, salmon, herring, sardines
- Egg yolk
- Mushrooms
- Foods that are fortified with vitamin D (cereals, milk, juices) are often inadequate to meet daily requirements of vitamin D
- The body can only absorb ~50% of the vitamin D that is naturally occurring in food
- Without enough vitamin D only ~10% of dietary calcium is absorbed and this only rises to 30-40% when vitamin D is in its normal limits
Vitamin D from food
| Food | Amount serving | Vitamin D3 (IU) |
|---|---|---|
| Cod liver oil | 1 teaspoon | 1300 |
| Wild fresh salmon | 100g | 650 |
| Farmed fresh salmon | 100g | 250 |
| Mackerel fish, cooked | 100g | 350 |
| Mackerel fish, canned | 100g | 250 |
| Sardines, canned | 100g | 300 |
| Tuna, canned | 100g | 240 |
| Liver, beef cooked | 100g | 50 |
| Egg yolk | 100g | 30 |
Who is most at risk of vitamin D deficiency?
- People with reduced exposure of skin to sunlight
- >65 years of age:
- Concentration of the cholesterol precursor of vitamin D (7-dehydrocholesterol) declines with age
- A 70-year-old has ~25% of the ability of a young healthy person to produce vitamin D from sunlight
- Despite this elderly are still capable of producing adequate amounts of vitamin D from sun exposure but just need longer time to achieve this
- Infants and children younger than 5 years
- Pregnant and breast feeding women
- Malnutrition and those not consuming adequate amounts of vitamin D containing foods
- Dark skin:
- Dark skinned people can require 5-10 times longer sun exposure than fair skinned people to produce the same amount of vitamin D
- Obesity:
- Vitamin D is fat soluble and is stored in body fat
- In obese people this vitamin D is stored more deeply and is less available to the body
- Blood level of 25-hydroxyvitamin D is ~20% less in obese people than normal weight
- For every 1 point rise on BMI (Body Mass Index) there is a 1.15% drop in 25-hydroxyvitamin D blood level
- Obese people with similar sunlight exposure to normal weight people produce the same amount of vitamin D but it is diluted into a greater volume of fat so the amount in the blood stream is less
- As a result of this dilution obese people need greater vitamin D supplementation to reach the desired blood levels
- Sedentary lifestyle
- People who work many hours indoors
- Conditions that reduce absorption of vitamin D in the gastrointestinal tract:
- Inflammatory bowel disease (Crohn’s, Ulcerative colitis)
- Pancreatitis
- Short bowel syndrome (either part of the small intestine has been removed, or born with short sections of it)
- Bariatric surgery
- Liver failure
- Kidney failure
- Medications that affect vitamin D metabolism e.g. antiepileptics, long term steroids
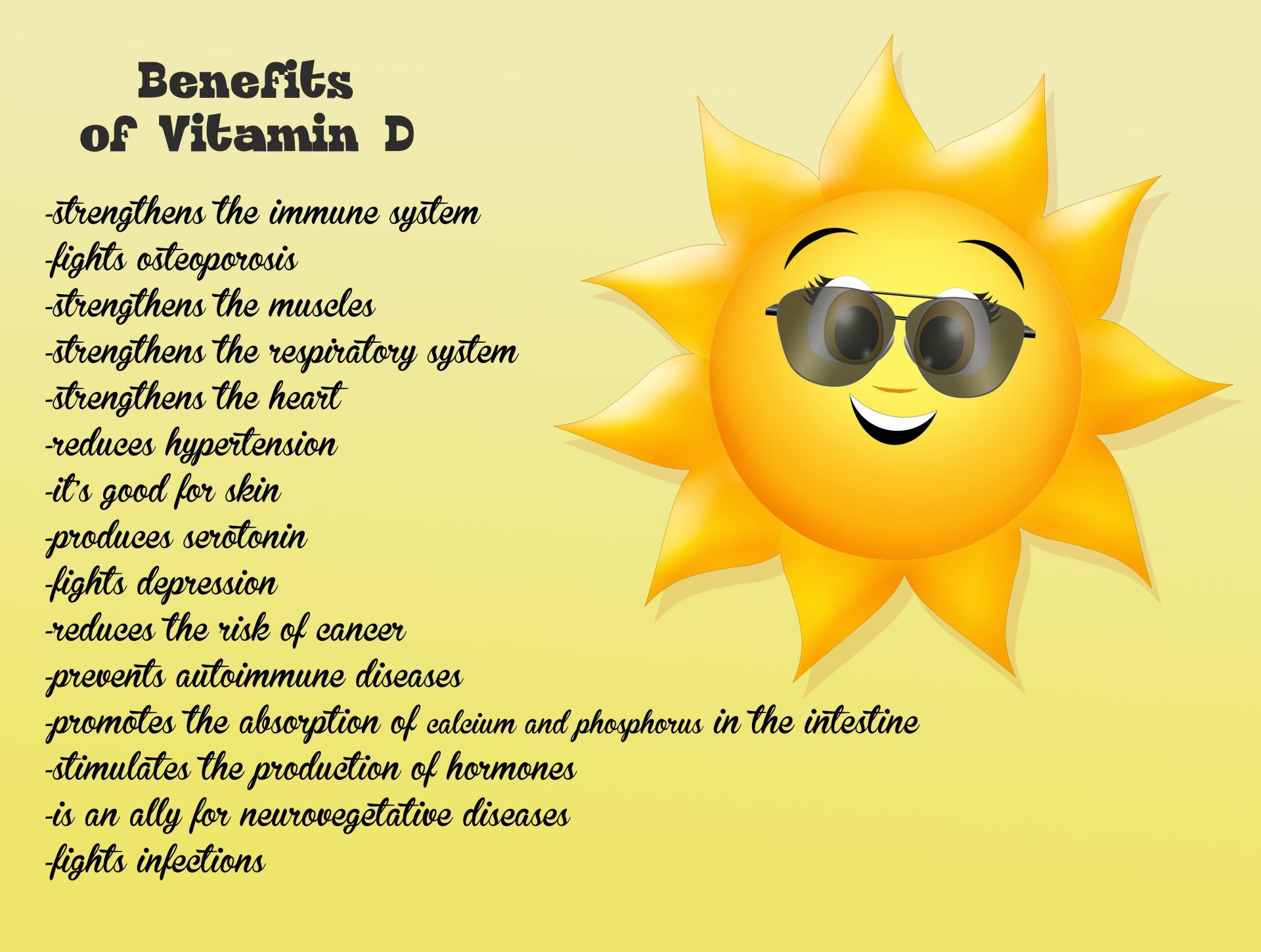
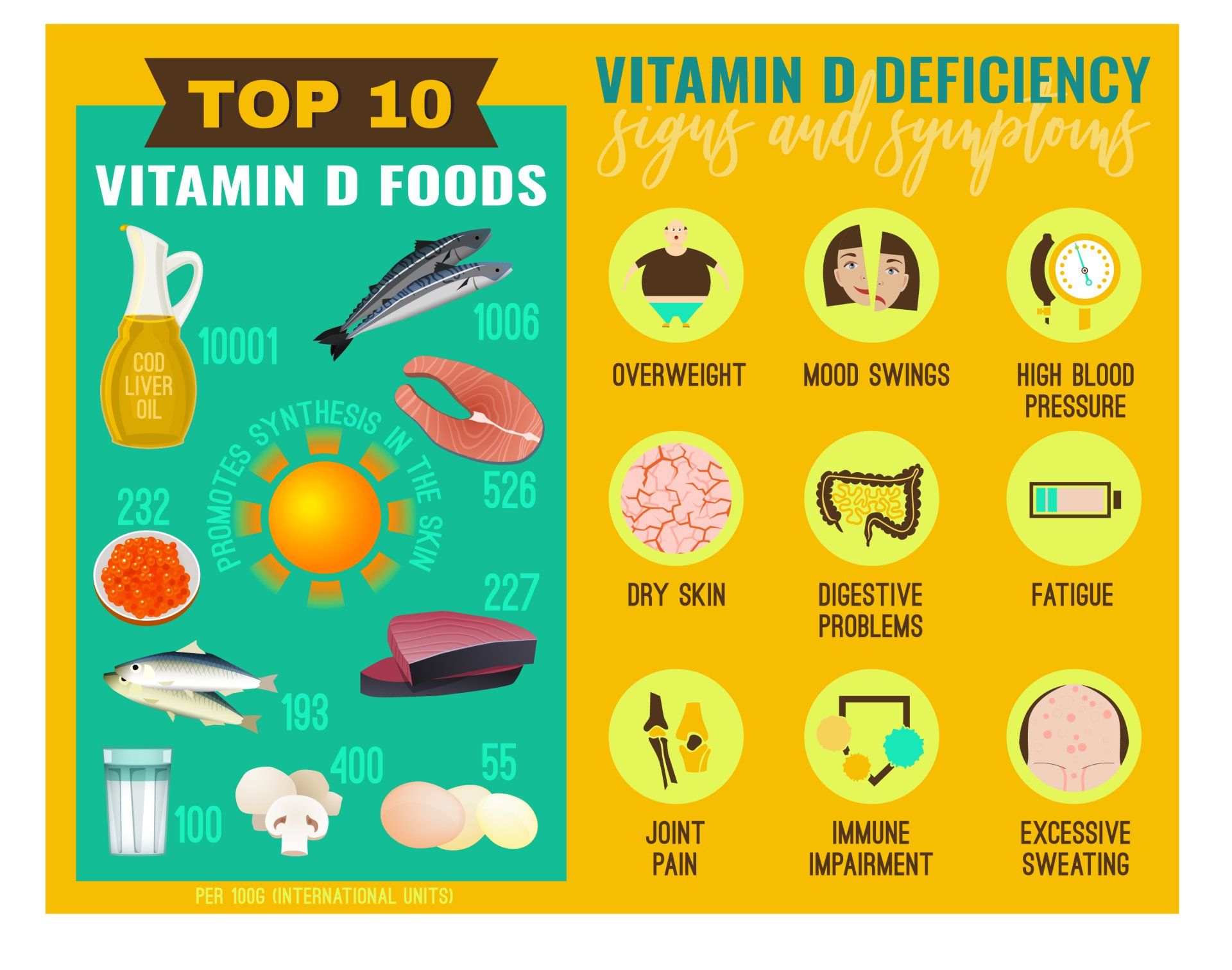
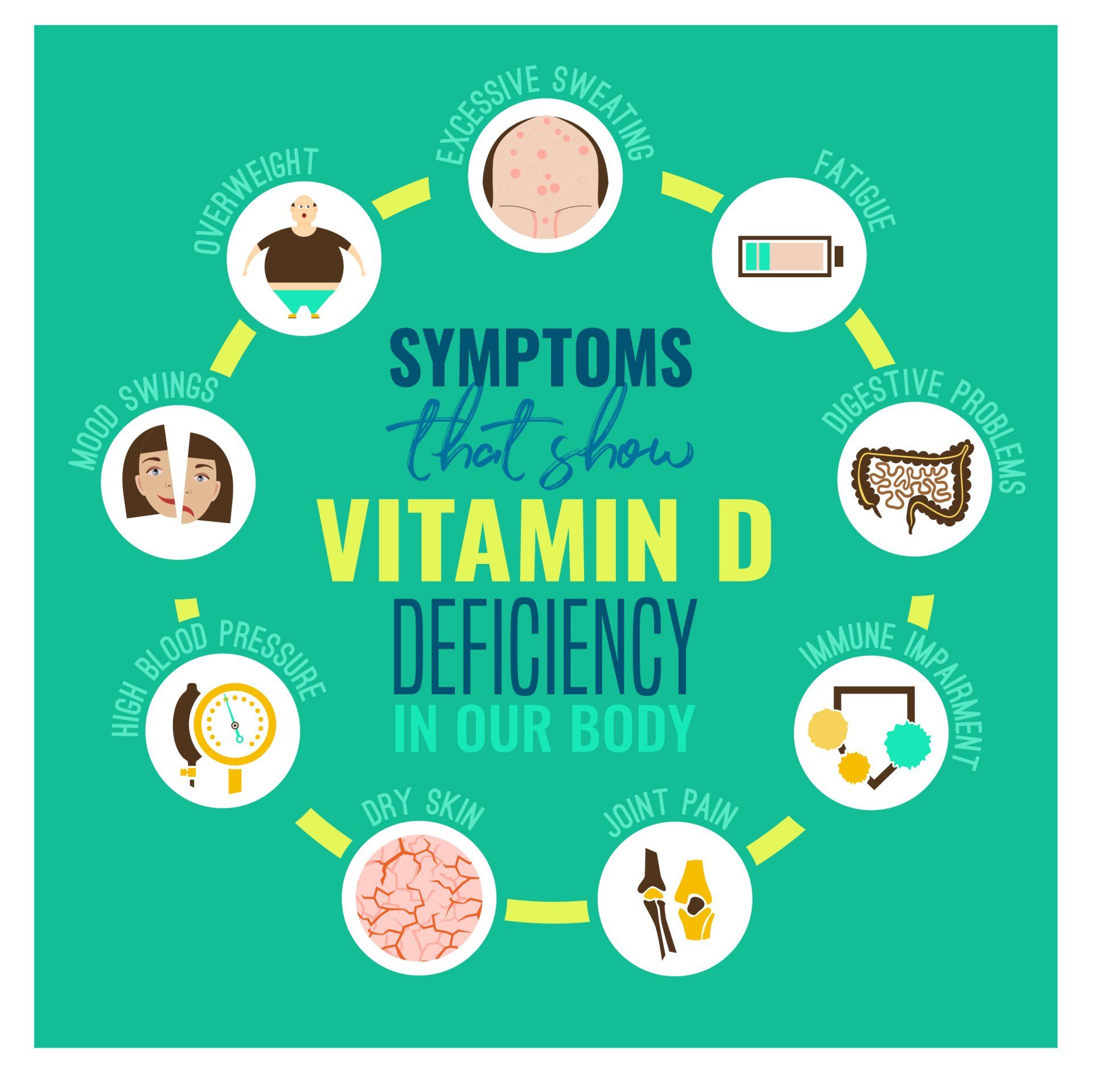
What are the benefits of vitamin D?
- Vitamin D has been shown to have a protective effect against the following conditions which have been noted to be at higher risk of getting them when there is vitamin D deficiency:
- Numerous musculoskeletal benefits (see below)
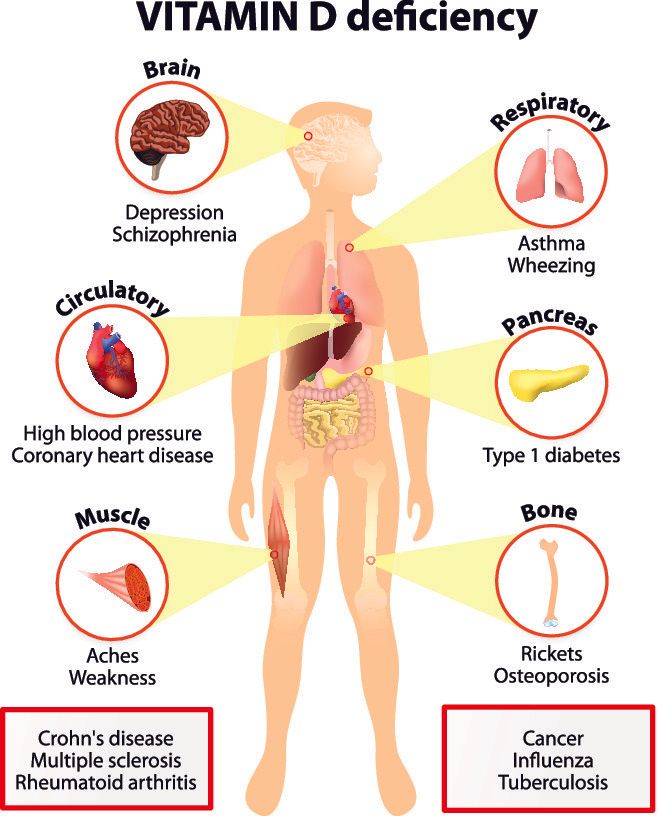
- inflammatory and autoimmune diseases such as:
- Diabetes mellitus (both type 1 and 2)
- Multiple sclerosis
- Rheumatoid arthritis
- Sjogren syndrome
- Colds and flu
- Periodontal disease: a leading cause of tooth loss in older people
- Cardiovascular disease:
- Heart attack
- Hypertension
- Heart failure
- Peripheral vascular disease
- Cancers:
- Colorectal
- Breast
- Ovarian
- Prostate
- Oesophageal
- Mental health problems:
- Depression
- Seasonal Affective Disorder (SAD)
- Dementia
- Schizophrenia
- Pregnancy:
- Increased risk of pre-eclampsia and diabetes during pregnancy
The role of vitamin D on musculoskeletal health
- Low vitamin D results in reduced absorption of calcium and phosphorus which are essential minerals for bone strength
- Low bone mineralisation leads to softening and weakening of bones:
- This is termed rickets when it occurs in children
- This is termed osteomalacia when it occurs in adults
- Vitamin D has been shown to help reduce bone fracture risk in two different ways:
- Reduces risk of fall
- Increasing bone density
- Vitamin D reduces risk of:
- Falls by 19%
- Hip fracture by 18%
- Non-vertebral fracture by 20%
- Hip by 19%
- The benefits of vitamin D are dose dependent:
- Reduced risk of falls was seen with doses greater than 700IU per day
- Reduced risk of fractures was seen with doses greater than 400IU per day
- No improvement in risk of fracture has been found for doses lower than 400IU
- The level of 25-hydroxyvitamin D in the blood stream was shown to have an impact on the extent of the benefit from vitamin D:
- Reduction of risk of falls was seen with levels at least 60nmol/litre (24ng/ml)
- Reduction of fracture risk was seen with levels at least 75nmol/litre (30ng/ml)
- The magnitude of the benefit for both increased with higher 25-hydroxyvitamin D levels in the bloodstream
- Muscle weakness is closely associated with falling and risk of fracture
- Vitamin D supplementation in the elderly has been shown to:
- Increase muscle strength
- Improve balance
- Reduce risk of falling
- Improvement in walking distance
- 30% of people who have sustained a fracture secondary to a fall develop a fear of falling that results in:
- Self-restriction of activities
- Decreased quality of life
- 400IU of vitamin daily has been shown to reduce risk of:
- Rheumatoid arthritis by 40%
- Multiple sclerosis by 40%
- Vitamin D deficiency leads to a myopathy characterised by:
- Proximal muscle weakness
- Widespread muscle pain
- Gait impairment (difficulty walking)
- Muscle impairment starts even before the occurrence of adverse effect on bone
- Proximal muscle weakness:
- Weakness of the muscles in the shoulders and hips
- 30% of patients with vitamin D deficiency present with proximal muscle weakness before changes are seen in the bloodstream
- Therefore, patients who present with proximal muscle weakness should consider vitamin D and calcium supplementation
Vitamin D status of athletes
- Whilst the effect of vitamin D on sports performance in athletes is still an area requiring more research, so far there have been some positive indications of its impact
- The level of 25-hydoxyvitamin D was found to be linked to jump height, jump velocity and power in adolescent females
- Positive correlation has been found between 25-hydroxyvitamin D with maximal oxygen uptake (VO2max) which is in indictor of aerobic fitness
- Greater gains on sport performance are made if the athlete has a lower 25-hydroxyvitamin D level prior to treatment and the gains are maximised when this level reaches >100nmol/l (40ng/ml)
- Vitamin D deficiency can result in reduction in the number and size of Type II (fast twitch) muscle fibres in the elderly population which is reversed with correction of vitamin D levels
- 25-hydroxyvitamin D level below 30ng/mL significantly increases the risk of stress fracture:
- 10-30% of track and field athletes are reported to have stress fractures
- More common in women
- Common cause of military recruits failing to complete training
- Even outdoor athletes have been found to be vitamin D insufficient
- Many outdoor athletes train early in the morning or late at night as they avoid peak sunlight hours
- Various studies have shown that athletes in sunnier countries have unacceptably high rates of vitamin D deficiency and insufficiency
Vitamin D levels in various athletes
| Athlete | Vitamin D Status |
|---|---|
| UK professional athlete | 60% deficient |
| Israeli indoor athletes | 73% insufficient |
| USA endurance runners | 42% insufficient |
| 11% deficient | |
| Australian gymnasts | 33% insufficient |
| Middle Eastern sportsmen | 32% insufficient |
| 58% deficient | |
| Finnish military recruits | 39% deficient |
The role of sunlight
- There are three types of ultraviolet radiation (UVR) coming from the sun and they are classified according to their wavelength:
- UVA:
- Long wavelength
- 95% of UV radiation reaching the Earth
- The most penetrable type of UVR and causing the most damage to the skin
- Sunscreens are less effective at blocking it
- UVB:
- Medium wavelength
- Most UVB is filtered by the atmosphere
- Biologically active and is the one responsible for Vitamin D synthesis
- Sunscreens can block it (higher the SPF the better the block)
- UVC:
- Short wavelength
- The most damaging type of UVR
- Filtered by the Earth’s atmosphere so doesn’t reach Earth’s surface
- A light skinned individual can produce 10,000 to 20,000IU in 15 minutes of unprotected sun exposure
- Interestingly the highest levels of vitamin D are found in farmers and lifeguards both of which involve many hours outdoors
Factors that affect UVR reaching Earth
- Time of day:
- At noon the sun is directly above and takes the shortest path to reach the Earth’s surface so this is the maximum time for UVR and therefore vitamin D synthesis
- There is a 4 hour window around noon during which time the UV rays are strong
- During early morning and late afternoon the sun’s rays reach Earth at a greater angle so more of the rays are absorbed by the atmosphere and less reach the Earth
- Time of the year:
- The angle the sunrays take to reach the Earth changes with the seasons
- This affects the distance they need to travel and the shorter it is, the greater the amount of UVR that reaches Earth
- Summer therefore provides the greatest exposure to UVR and winter the least
- Latitude:
- UV levels are highest closest to the equator as the sun’s rays travel the least distance through the atmosphere
- Evidence shows that latitudes greater than 37 degrees from the equator are an increased risk for lower vitamin D synthesis from sunlight
- Below are a list of cities and their latitudes for ease of reference:
- Abu Dhabi: 24
- Miami: 25
- Cairo: 30
- Los Angeles, Sydney: 34
- Las Vegas, Rhodes, Santorini: 35
- Athens: 37.98 degrees
- Beijing, Valencia: 39
- Thessaloniki, New York, Madrid: 40
- Montreal, Milan, Belgrade: 45
- Paris, Munich: 48
- London: 51
- Edinburgh, Moscow: 55
- Altitude:
- The greater the vertical height from sea level the less atmosphere exists to absorb the sunlight
- For every 1km height, the UV levels under clear skies increase by ~7%
- Atmospheric conditions:
- Clouds:
- Cloud cover can affect UVR penetration but this depends on the type of cloud and how deep it is in the atmosphere
- A fully cloudy day can reduce the UV rays by 70-90%
- A thin or partly cloudy day can actually increase UVR exposure by 20% by having a mirror effect
- The thinner the ozone the less UVR is absorbed
- The greater the air pollution the more UVR are absorbed
- Ground reflection:
- Various surfaces can add to the UV exposure through reflection
- Grass, soil, water provide <10% reflection
- Sand 15% reflection
- Snow can through reflection can nearly double UV exposure
Factors that affect ability to make vitamin D from sunlight
- Skin pigmentation:
- There are 6 different types of skin based on their ability to tan (Fitzpatrick skin pigmentation scale)
- As the skin gets darker the ability to synthesise vitamin D reduces but there is greater protection against skin cancer
- Amount of skin exposed:
- The more skin that is exposed the greater the potential for vitamin D synthesis
- Posture of the body under the sun:
- Greatest exposure is when the skin is 90 degrees to the sunrays i.e. lying horizontally at noon
- Standing up reduces the amount of skin exposed to the sunlight
- Surroundings:
- Presence of objects providing shade e.g. umbrellas
- Urban areas have buildings that reduce sunrays reaching ground level compared to open rural areas
- Sun exposure:
- There is a lot of misconception regarding how to best produce vitamin D from sunlight
- Many people avoid exposure to sunlight around noon and instead spend long time sunbathing outside of these hours
- Literature shows that the best time to absorb UVB are for a few minutes at lunchtime
- Outside of this time, UVB rays reduce in intensity whilst UVA rays continue to reach Earth and so lengthy sun exposure in late afternoon and early morning actually increases risk to skin cancer whilst offering less vitamin D benefits compared to 5-10 minutes at lunchtime (lighter skin need less, darker skin needs a lot longer)
- An easy indication of when sunbathing does not produce vitamin D is when the shadow of someone who is standing is longer than what they are in height
Fitzpatrick skin pigmentation scale
| Skin Type | Appearance | Skin reaction to UV light |
|---|---|---|
| Type 1 | Pale to very fair skin | Burns easily |
| Red or blond hair | Never tans | |
| Light coloured eyes (blue/green) | Highest risk of skin cancer | |
| Type 2 | Fair skin | Burns easily |
| Light hair | Rarely tans | |
| Light eyes | High risk of skin cancer | |
| Northern European origin e.g. Scandinavians, Celts | ||
| Type 3 | Light brown skin | Sometimes burns |
| Medium to dark hair | Tans gradually | |
| Mediterranean and Middle East origin | ||
| Type 4 | Medium brown skin | Hardly ever burns |
| Dark hair and eyes | Tans easily | |
| East Asian origin e.g. Chinese, Japanese | Scars easily | |
| Type 5 | Dark brown skin | Skin darkens but very rarely burns |
| Dark hair | High risk of scarring | |
| Dark eyes | Low risk of aging and skin damage from sun exposure | |
| Some people of African origin | ||
| South East Asians e.g. Indians, Pakistanis | ||
| Type 6 | Very dark skin | Tans easily but never burns |
| Dark hair | High risk of scarring | |
| Dark eyes | Low risk of aging and skin damage from sun exposure | |
| African origin and Aborigines |
Vitamin D levels and skin pigmentation
- Vitamin D insufficiency is more common in African Americans than Caucasians
- Dense skin pigmentation can reduce vitamin D production by >90%
- The darker pigmentation is due to the higher concentration of melanin in the skin which absorbs ultraviolet light and reduces the amount that reaches the deeper layers of skin thus protecting it from UVR damage
- Unfortunately the deeper layers is where vitamin D is synthesised from UV light
- African Americans are also noted to have lower dietary intake of vitamin D perhaps due to higher rate of lactose intolerance leading to reduced intake of milk products and cereals fortified with vitamin D
- Darker skinned people whilst they are more protected more from skin cancers than fair skinned people, they would need to expose themselves for longer duration to sunlight to synthesise the same amount of vitamin D
- However African Americans have lower rates of osteoporotic fractures:
- A 65 year old Caucasian woman has an 11% chance of a hip fracture by the time she is 80 compared to only 4% of an African American woman
- It isn’t entirely clear why this difference is noticed despite the lower vitamin D levels in African Americans but it is thought to be due to higher bone mineral density early in life
The Mediterranean paradox
- Despite countries in Southern Europe having more abundant UVB sunlight, they have been shown to have higher prevalence of vitamin D deficiency compared to countries in central Europe – the so called Mediterranean paradox
- This has been shown to be the case in Greece as well and reasons for the lower than expected vitamin D are:
- Higher melanin concentration in the skin
- Avoidance of sunlight exposure and use of sunscreen
- Reduced outdoor activity especially in cities compared to rural regions
- Reduced consumption of food rich in vitamin D
- Absence of vitamin D fortified foods (except for children’s and infants’ milk)
- Many countries like Greece do show seasonal variation whereby there are lower vitamin D levels occur post-winter and the highest post-summer
- Vitamin D produced from sunlight is stored in the body 2-3 times longer than from oral supplements
- There are no reports of vitamin D toxicity due to excessive sun exposure and the reason being that the previtamin D compounds that are produced have very little effect on calcium levels
The Middle East is plagued with low vitamin D
- Countries in the Middle East with an abundancy of UV light have some of the lowest levels of vitamin D worldwide:
- Limited sun exposure in these countries can be due to cultural practices
- Very hot climate makes it difficult to sunbathe under the sun
- Dark skin colour
- 10-60% of mothers and 40-80% of neonates are found to have negligible levels (0-10 ng/ml)
- Adults are similarly affected with rates of 30-80%
- Interestingly immigrants from the middle East to Western countries continue to have some of the lowest levels of vitamin D in that country
Does sunscreen reduce ability to make vitamin D?
- Skin cancer is the most commonly occurring cancer in the white population
- Sunscreen helps protect skin from the harmful effects of UVR and helps reduce risk of:
- Squamous cell carcinoma by 40%
- Melanoma by 50%
- Premature skin ageing by 24%
- Whilst there have been some reports raising concerns over the negative impact of use of sunscreen on vitamin D production, evidence is lacking to support this
- Areas of skin that have less cholesterol under them produce less vitamin D i.e. face, hands, and feet:
- It is particularly important to put sunscreen to face and wear a hat to protect it from sun exposure
What would be the optimal way to produce vitamin D from sunshine?
- The latest guidelines suggest 5-15 min/day of sun exposure at midday would produce enough daily vitamin D and this can be followed by application of a broad spectrum sunscreen with an SPF of at least 15:
- Darker skinned individuals are likely to need longer
- This approach helps to maximise the benefits from UVB rays in the shortest possible time whilst minimising the damaging effect from UVA rays
- Sunbathing for longer periods especially without sunscreen increases risk of skin cancer whilst being less beneficial for vitamin D production
Vitamin D insufficiency in schoolchildren
- Studies have shown the prevalence of vitamin D insufficiency in schoolchildren living in Europe to be 25-63%
- In large study in Greece this was found to be 53% and is higher than most other European nations:
- Girls are significantly at higher risk
- More prevalent in areas in and around cities rather than rural areas:
- This has been noted in studies of other countries as well and thought to be due to more open spaces, more outdoor activities, less tall buildings and clearer skies in rural areas
- Children who have taken 2000IU of vitamin D daily since 1st year of age and were followed up for 25 years had 80% reduced risk of developing type 1 diabetes:
- In the same study children who were vitamin D deficient, had 4 times risk of developing type 1 diabetes later in life
- In Greece the prevalence of vitamin D insufficiency is 60% for obese and 50% for overweight children:
- This is the critical time period to build strong bones and failure to maximise this opportunity due to vitamin D deficiency poses a significant risk of osteoporosis and fractures later in life
- Whilst the prevalence of vitamin D insufficiency among children and adolescents in Greece is better than some other countries (96% in Germany, 78% in USA) it is still of great concern and there should be a nationwide campaign to improve on this easily modifiable health risk
Vitamin D toxicity
- Vitamin D toxicity is extremely rare
- The resulting increased calcium concentration is the main worry
- When hypercalcaemia is mild it can be asymptomatic but more severe levels can present with:
- Nausea
- Dehydration, excessive thirst and frequent urination
- Abdominal pain
- Constipation
- Kidney stones
- Bone pain and muscle weakness
- Hypertension
- Anxiety and depression
- Confusion, lethargy and fatigue
- Once again there isn’t widespread agreement on what toxicity levels are, simply because people have different sensitivities to vitamin D
- Most report this to be 250nmol/l (100ng/ml) but there are rare cases happening below this level
- That is why it is important to analyse the calcium and vitamin D levels as well as patient’s symptoms
- Whilst the upper daily safe limit for adults has been set at 10,000IU/day it would take months or even years for this to become toxic
- One report showed no cases of toxicity with daily intake of 30,000IU/day for an extended period of time
Seasonal Affective Disorder (SAD)
- A type of depression caused by the changes in the seasons
- It usually starts around the same time each year, most commonly during autumn and goes into the winter months and goes away when the sunnier days arrive in spring and summer
- Symptoms:
- Feeling depressed
- Low energy and tiredness
- Oversleeping
- Weight gain and craving for foods high in carbohydrates
- Difficulty concentrating
- Low self esteem
- If severe can lead to thoughts of suicide
- Risk of SAD is increased if:
- There is family history of SAD or other form of depression
- Personal history of depression
- Reduced sunlight exposure which is more common in people living far from the equator
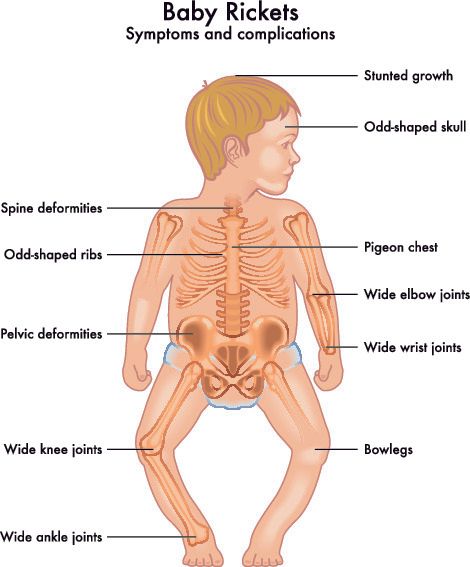
Rickets
- Rickets is softening and weakening of the bones in children due to poor mineralisation of the bones
- It is caused by deficiency in vitamin D, calcium or phosphorus
- It can lead to deformation of a child’s bones and making them prone to fractures
- Due to the increased calcium requirements of children, insufficient intake can lead to rickets:
- Rickets is most commonly seen between 6 and 36 months of age
- During this period there is a rapid growth spurt
- Whilst rickets is largely eradicated in Western countries it is still found in dark skinned communities that have migrated to latitudes far away from the equator
- Some of the highest rates of rickets is found in the Middle East despite the abundance of sunlight
- This is largely due to:
- Limited sun exposure
- Cultural practices
- Darker skin colour
- Low calcium intake
Presentation
- Pain:
- The child may be reluctant to walk due to bone pain
- When they walk it may look different (called waddling gait)
- Pain in legs, pelvis and spine
- Musculoskeletal problems:
- Thickening of various joints:
- Ankle, wrists, knees
- Characteristic bowing of the legs (varus deformity)
- Softening of the skull bones
- Muscle weakness
- Poor growth and development:
- Child will end up being shorter than average
- Dental problems:
- Defective or weak tooth enamel
- Increased risk of tooth cavities
Causes
- Low vitamin D:
- Inadequate oral intake
- Inability to absorb vitamin D despite adequate intake:
- This is hereditary and runs in families
- Mother’s vitamin D deficiency during breastfeeding
- Exclusive breast feeding: as this doesn’t have any vitamin D
- Northern latitudes
- Premature birth
Osteomalacia
- Osteomalacia is softening and weakening of bones like rickets but for adults
- Most often caused by severe vitamin D deficiency
- Increases the risk of fractures in adults
What is the difference between osteomalacia and osteoporosis?
- In osteomalacia there is normal bone density but inadequate bone mineralisation:
- Bone mineralisation is the process of addition of calcium and phosphorus containing complexes (called hydroxyapatite) to the bone structure and gives it additional strength
- On the other hand, osteoporosis has normal bone mineralisation but low bone density:
- This reduced bone density in osteoporosis makes the bones weaker and susceptible to fractures
Causes
- Osteomalacia is caused by any process that reduces bone mineralisation
- Bone mineralisation requires adequate intake of calcium, phosphorus and vitamin D
- Vitamin D deficiency is the most common cause
- The Middle East and north Africa has one of the highest rates of rickets and osteomalacia in the world
Symptoms
- In the early stages there are often no symptoms
- As it gets more severe it can present with:
- Dull achy bone pain especially in lower back, pelvis, hips, legs and ribs
- Pain is typically not completely relieved by rest
- Pain can be worse at night and on pressure upon the bones
Further relevant information can be found on:

Introduction Cubital Tunnel Syndrome occurs when the ulnar nerve is compressed within a tunnel on the inner (medial) side of the elbow just behind the bony prominence of the inner aspect of the elbow called the medial epicondyle Cubital Tunnel Syndrome is the second most common cause of peripheral nerve compression: The most common one being carpal tunnel syndrome (compression of the median nerve at the wrist) The ulnar nerve is one of the three main nerves of the upper limb: The other two nerves of the upper limb are the median nerve and the radial nerve The ulnar nerve travels from the neck past the elbow and wrist and into the hand: Along the way it travels past some narrow areas where it can be constricted and cause symptoms for the patient The most common site of ulnar nerve compression is in the cubital tunnel at the elbow The second most common site is in Guyon’s canal in the hand When someone accidentally hits the inner side of the elbow (often termed hitting the funny bone) they get a sharp tingling sensation on the inner side of the elbow and forearm: This occurs because the ulnar nerve was hit at the site of the cubital tunnel where the nerve is close to the skin surface and therefore easily injured from outside forces
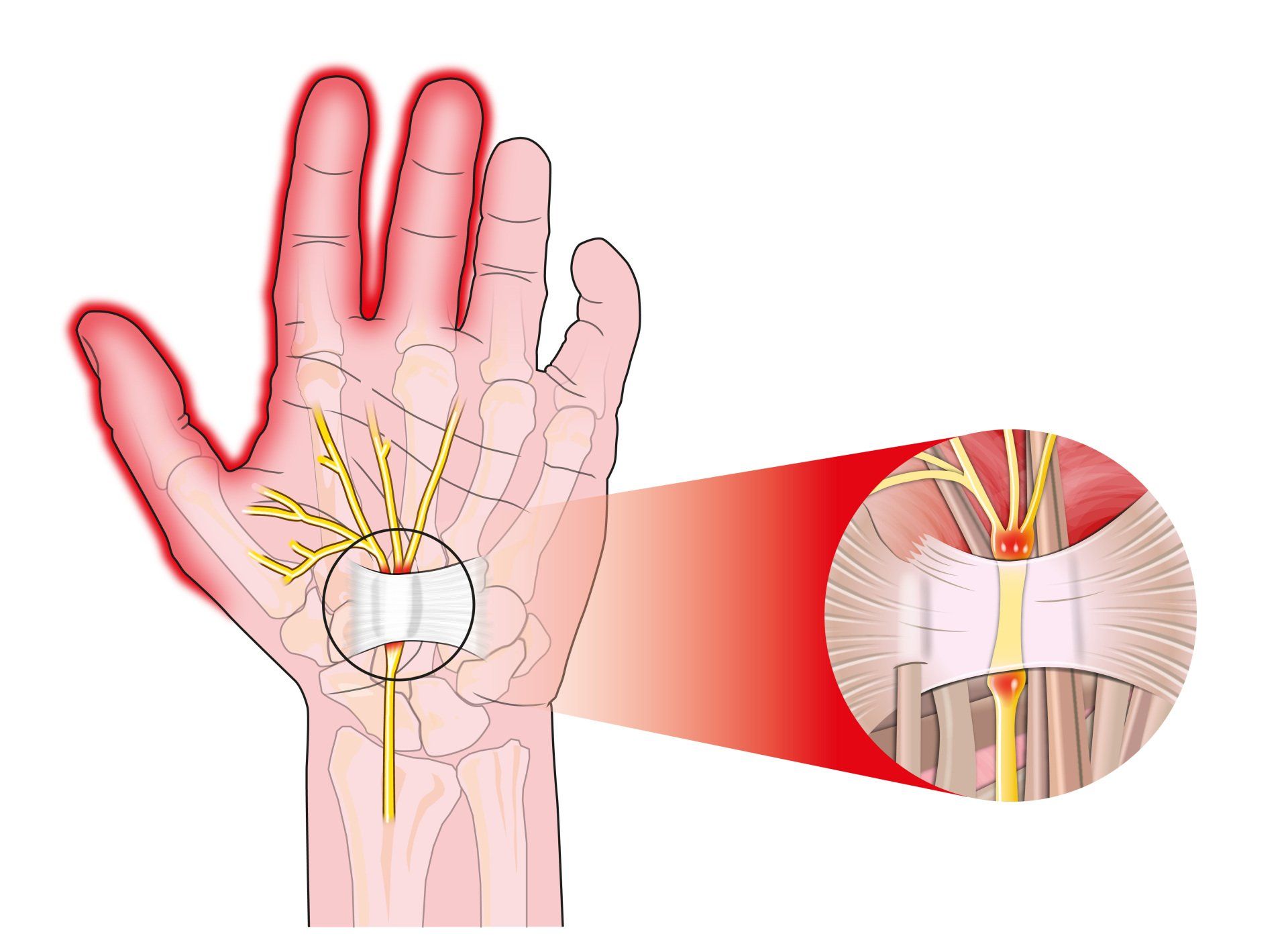
Introduction Carpal tunnel syndrome is a common condition that causes numbness, tingling and weakness in the hand specifically affecting the thumb, index and middle fingers: The little and ring fingers are not affected as they are supplied by another nerve called the ulnar nerve It is the commonest cause of peripheral nerve entrapment It is caused by compression of the median nerve as it passes from the forearm into the hand through a passage called carpal (i.e. wrist) tunnel The median nerve is one of three main nerves that supply the upper limb: The other two nerves are the ulnar nerve and the radial nerve
Introduction Tennis elbow (also known as lateral epicondylitis) is an overuse injury of the forearm tendons that originate over the lateral epicondyle of the humerus (bony prominence on the outside of the elbow) and act to bring the wrist backward away from the palm Whilst tennis players are particular prone to this condition it does not occur exclusively to them

Introduction This term is also known as repetitive motion or stress injury and occurs as a result of carrying out the same motion repeatedly over time causing injury to muscles and tendons It is associated with repetitive tasks, sustained or awkward position, forceful exertion, vibration or compressive forces It can affect almost any joint in the body Most commonly affected areas are hands, wrists, shoulders and neck It is thought to affect 5-10% of the general population but can be as high as 20-40% in specific working populations