Meniscal Tears
Overview
- Meniscal tears are the most common injury presenting to a knee surgeon
What are the main types of meniscal tears:
- Two main types of tears are:
- Acute tear:
- due to traumatic event commonly while the knee is flexed, loaded and twisted
- more common in younger active patients
- Degenerate tear:
- Occur in the elderly
- In MRI scans of people over 65 years they are found in 67% of if they have no symptoms and over 90% in those with symptoms
- Can occur with no history of trauma or from minor event such as kneeling, squatting, getting out of the car
- As meniscus ages it becomes weaker, more friable, less elastic and more prone to tears
How are meniscal tears described?
- Meniscal tears can be described according to their appearance:
- Intrasubstance meniscal tear:
- This occurs when there is increased signal in the MRI scan within the substance of the meniscus suggestive of an injury but the signal does not reach the surface of the meniscus and at arthroscopy there is no visible tear
- They are often early sign of degenerative change to meniscal tissue
- These are managed conservatively
- Incomplete meniscal tear:
- This is a common finding whereby there is a visible tear on one side of the meniscus surfaced but it doesn’t go fully through to the other side
- These can be managed conservatively
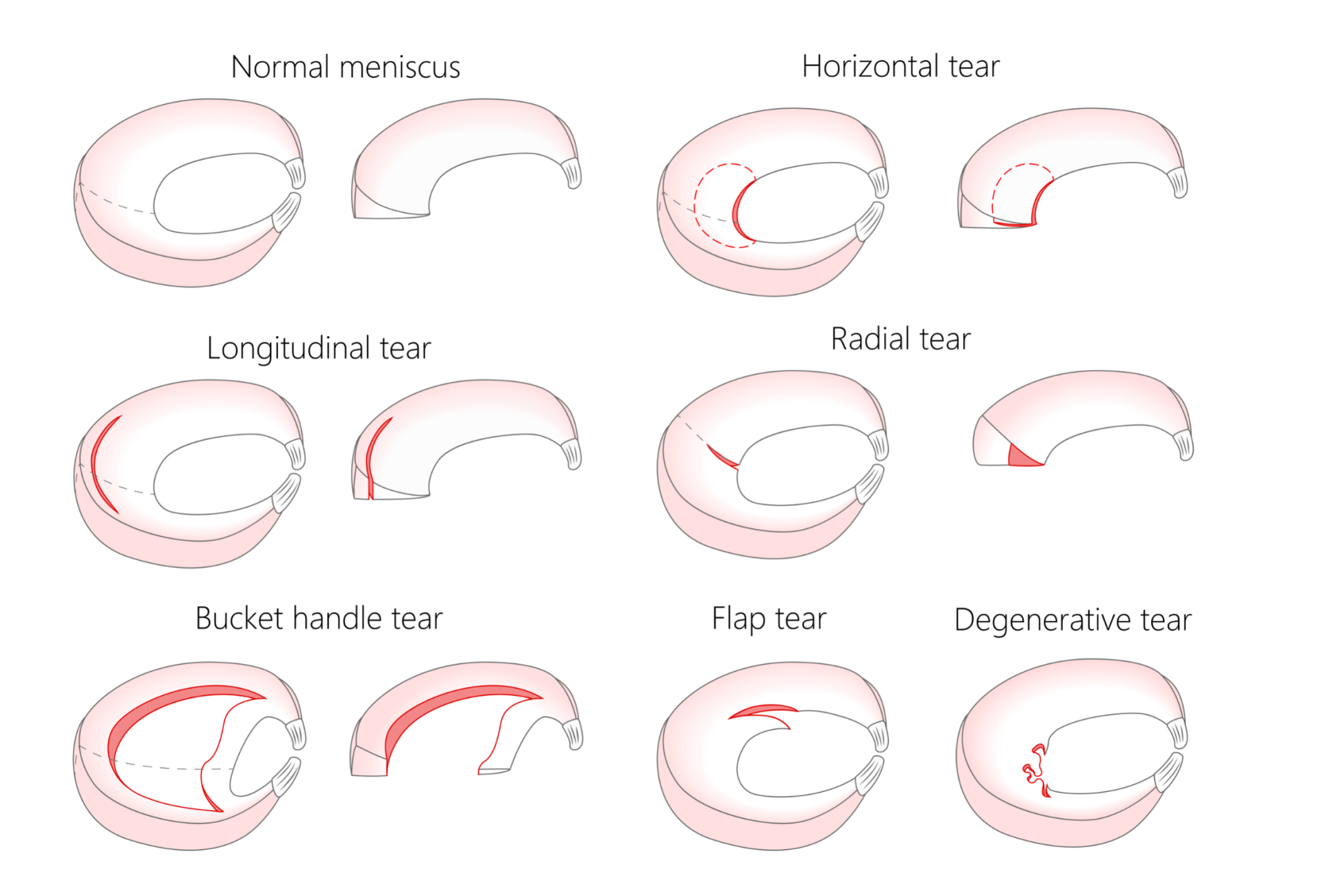
- Radial meniscal tear:
- Most common type of meniscal tear
- They are short tears that extend from the inner margin of the meniscus to the periphery
- They have little capacity to heal unless they involve the peripheral (red-red) zone
- They often need arthroscopic trimming of the damaged portion
- Horizontal meniscal tear:
- Tear in the horizontal plane and is most amenable to repair
- The ones located more peripherally have good potential for healing unlike the more centrally located ones that often need debridement
- Longitudinal meniscal tear:
- Vertically orientated tear which is parallel to the periphery
- Bucket handle meniscal tear:
- more extensive version of the longitudinal tear
- Usually traumatic in younger athletes
- It takes its name from the motion of a bucket handle that can rotate and flip and when it displaced to the middle of the knee it causes locking (inability to get the knee straight)
- These require prompt surgical intervention
- In experienced hands an increasing number can be repaired pending the quality of the remaining tissue and how reducible and fresh the tear is
- Meniscal flap tear (also termed parrot beak tear):
- These can be painful if the catch as the knee moves and can extend over time
- Complex meniscal tear:
- Combination of various tear patterns often involving radial and horizontal components
- They are not repairable and if symptomatic may require trimming
- Complete meniscal tear:
- This is when the tear goes across the full width of the meniscus
- It defunctions the meniscus and is a serious injury
What is a ramp lesion (meniscocapsular tear):
- A meniscal ramp lesion is a longitudinal tear of the peripheral attachment of the posterior horn of the meniscus (medial meniscus affected more commonly than the lateral meniscus) to the capsule
- The substance of the meniscus itself is in tact but the meniscus has detached itself from the knee capsule at the back (hence the name meniscocapsular tear)
- The attachment between the meniscus and the capsule is the second most important stabilising factor of the meniscus after its root (see below)
- The meniscal ramp lesion is an increasingly recognised injury particularly in the presence of an ACL tear
- Meniscal ramp lesions play a big role in the anteroposterior and rotational stability in ACL deficient knees and so it is imperative that they are actively looked for both in MRI scans and at the time of arthroscopy
- Failure to recognise and repair them in the presence of an ACL injury increases significantly the chances of the ACL reconstruction failing
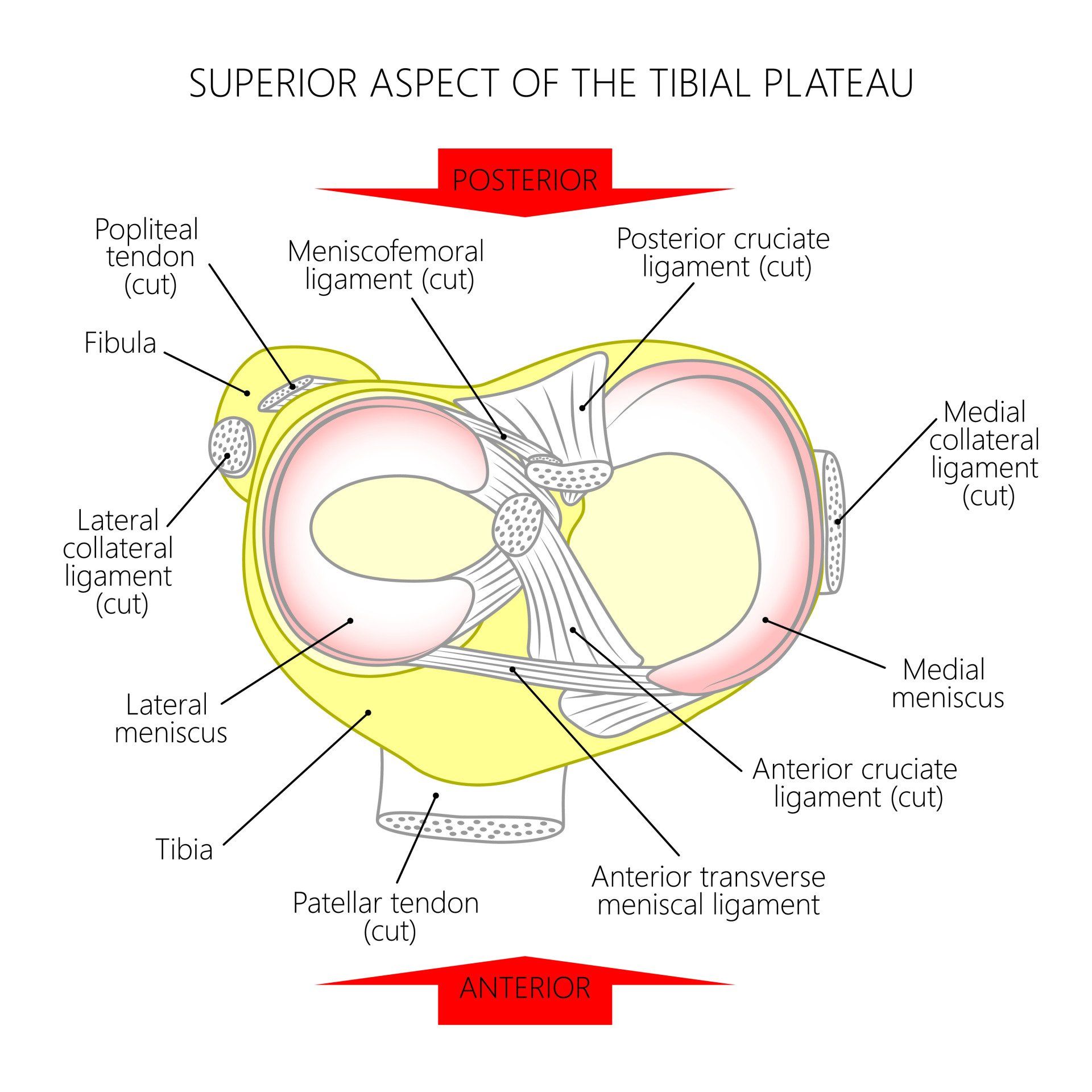
- Each meniscus is anchored to the underlying tibia via the anterior (front) and posterior (back) meniscal roots
- If either of the roots are torn it essentially defunctions the meniscus and leads to early osteoarthritis in that compartment
- Meniscal root tears are increasingly recognised and can be repaired by a specialist knee surgeon if they are caught early and the meniscal tissue is of sufficient quality and not friable
- Posterior root tears are more common than anterior
- Most root tears are degenerate in nature in the older population with no specific trigger or following minor traumatic event such as squatting
- The next commonest cause is traumatic particularly in the young and are associated with ACL injuries
- Posterior lateral meniscal root tears are 10 times more likely to occur with an ACL tear than posterior medial meniscal root tear and they provide significant stability to the knee in both front to back plane and rotational instability
- The posterior medial meniscus root tear occurs mostly (70%) in degenerate knees, particularly in women
- Tear of the posterior medial meniscal root is found in 80% of patients with SONK (Spontaneous Osteonecrosis of the Knee):
- SONK is when the bone around the knee (mostly the medial femoral condyle at 94%) starts to die off
- This can lead to the bone breaking off and the cartilage disintegrating and leads to osteoarthritis
- Risk factors for tear in the posterior medial meniscal root are increasing age, obesity, females and bow-shaped (varus) legs
How does the stability of a meniscal tear affect symptoms and outcome?
- A stable meniscal tear means it doesn’t displace as the knee moves and so it has a good chance to heal and be less symptomatic
- An unstable meniscal tear means it displaces (moves) as the knee moves and so it causes pain and symptoms if it is not surgically treated
Who gets meniscal tears?
- Can happen to anyone and not just those playing sport
Symptoms of a meniscal tear
- Pain:
- especially when twisting and turning and squatting
- usually sharp in nature
- well localised
- interferes with activities of daily living and participation in sports
- Swelling:
- Maximal swelling typically occurring many hours or a day later (as opposed to ACL injury which is within few hours)
- The swelling is moderate in size unlike a cruciate ligament injury where there is tense swelling
- Clicking
- Giving way:
- As the knee moves it can catch the torn part of the meniscus causing sharp pain which can trigger muscle
- Locking:
- The knee gets stuck and patients is unable to get the knee fully straight
- They may be able to eventually straighten the knee by bending or wiggling the leg
- This is very suggesting of an unstable meniscal tear getting caught between the articulating surfaces of the femur and tibia
- Hear of feel a pop:
- Meniscal root tears can mimic the sensation of a pop in the knee much like an ACL tear but the knee doesn’t swell up as rapidly or as much
When to seek urgent medical attention
- Locking:
- A knee is locked when a person is unable to fully straighten or bend their knee
- There are two types of locked knee:
- True locking:
- When there is a physical block to movement due to something getting stuck within the knee joint This can be caused by:
- Displaced meniscal tear
- Loose body (often cartilage or bone fragments)
- Patella dislocation
- Pseudolocking:
- Severe pain triggers muscles around knee to spasm, contract and prevent knee movement
Diagnosis
- History and examination of knee
- MRI scan is the investigation of choice:
- It can detect tears around 75-90% of the time meaning that a tear can exist with a normal MRI scan
- Helps diagnose other related pathology such as articular cartilage damage and ligament injuries
- Arthroscopy:
- Is the definitive method of assessing and treating meniscal tears as you can directly visualise and probe them with an instrument to assess them more accurately
Treatment of Meniscal Tears
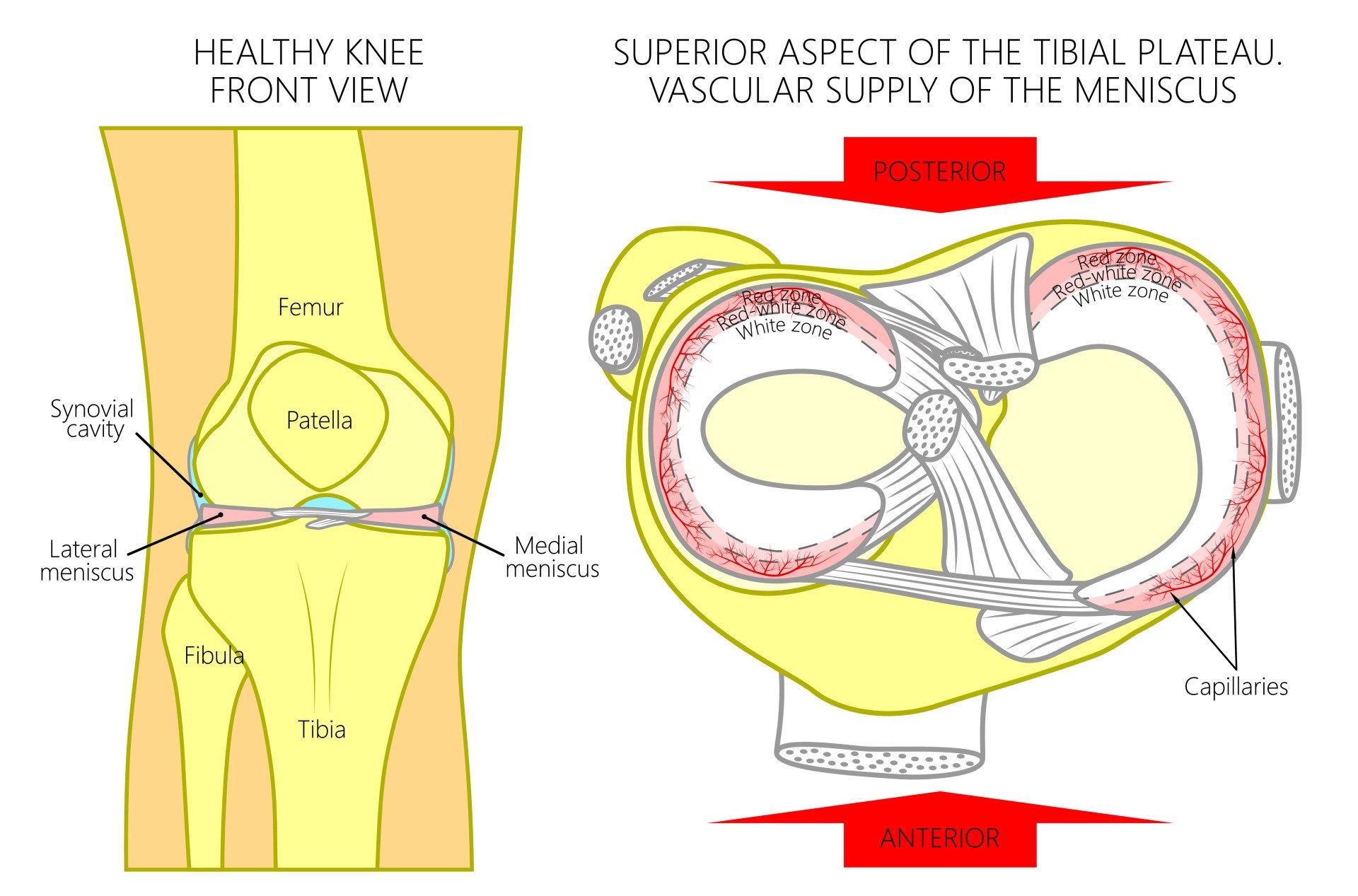
- Repair is most successful in younger patients, small tear, in the periphery where blood supply is best
- Repair of meniscus is even more successful in the event of ACL reconstruction at the same time
- However not all meniscal tears need surgery
- The degenerate meniscal tears in particular can be managed conservatively and after a few weeks the symptoms tend to subside
- As patients get older and physical demands and expectations decline a trial of conservative management can help avoid going through an operation
Treatment options for meniscal tears
- Factors that affect the treatment option for a meniscal tears are:
- Physical demands and expectations of the patient
- Age of the patient
- Additional injury within the knee
- Patient’s symptoms and whether conservative measures have failed after a period of time
- Size of tear
- Location of tear:
- how near it is to the vascular region of the meniscus
- Type of tear:
- not all tears are amenable to repair
- Quality of meniscal tissue:
- both the torn and the remaining part will determine if repair is feasible
- Presence and severity of arthritis
- Experience of surgeon in meniscal repair and the various techniques used to achieve optimal results
When is conservative management suitable for meniscal tears?
- Not all meniscal tears require an operation
- Small, stable tears can heal on their own
- Some tears cause no symptoms whilst other tears such as partial and degenerative can be observed for 2-3 months
- The goal is to provide pain relief and regain range of motion
- Pain relief with medications
- Swelling: treated with rest, ice, elevation, compression
- Avoid aggravating activities in particular twisting, pivoting, squatting
- Exercises to help maintain muscle strength whilst the is knee straight or only slightly flexed
- If symptoms persist after 6-12 weeks consider knee arthroscopy
When is operative treatment required for meniscal tears?
- Surgery for a meniscal tear is indicated if:
- A displaced tear that causes knee to lock (inability to go fully straight)
- ACL is also injured:
- This will make the knee even more unstable so the meniscus is unlikely to heal on its own
- High level athlete
- Symptoms are persistent and disabling for at least 2-3 months following appropriate conservative measures
What are the indications for meniscal repair;
- Meniscal repair is more successful in :
- Younger patients (the upper age limit is 40) because there is better blood supply which is required for the healing of the repair
- Peripheral tears (red-red zone) rather than central tears (white-white zone) because the periphery of the meniscus has better blood supply than the central part
- Fresh tears rather than chronic ones
- Tears that are in a single plane rather than multidirectional