Total Knee Replacement (TKR)
Total Knee Replacement (TKR)
What is a TKR?
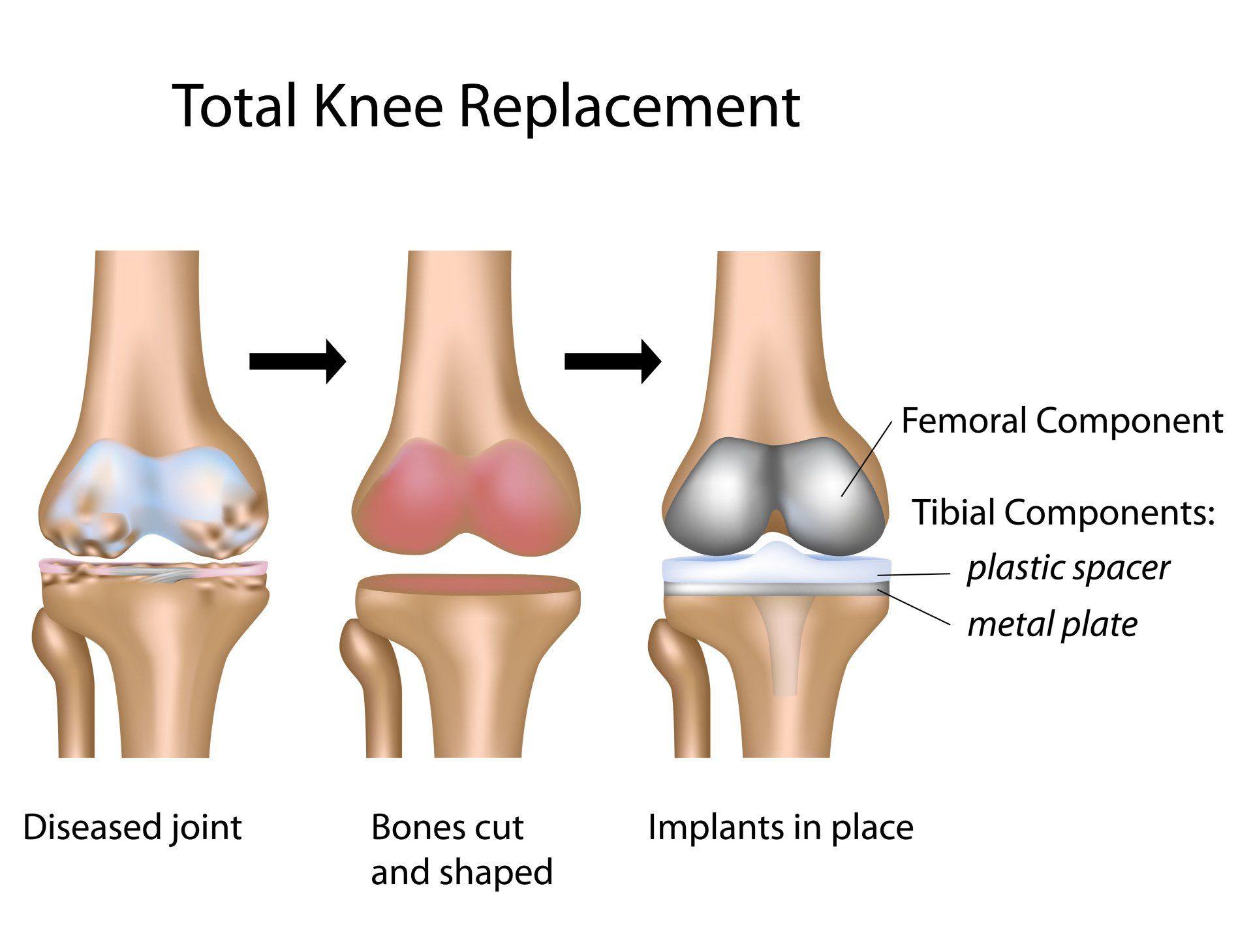
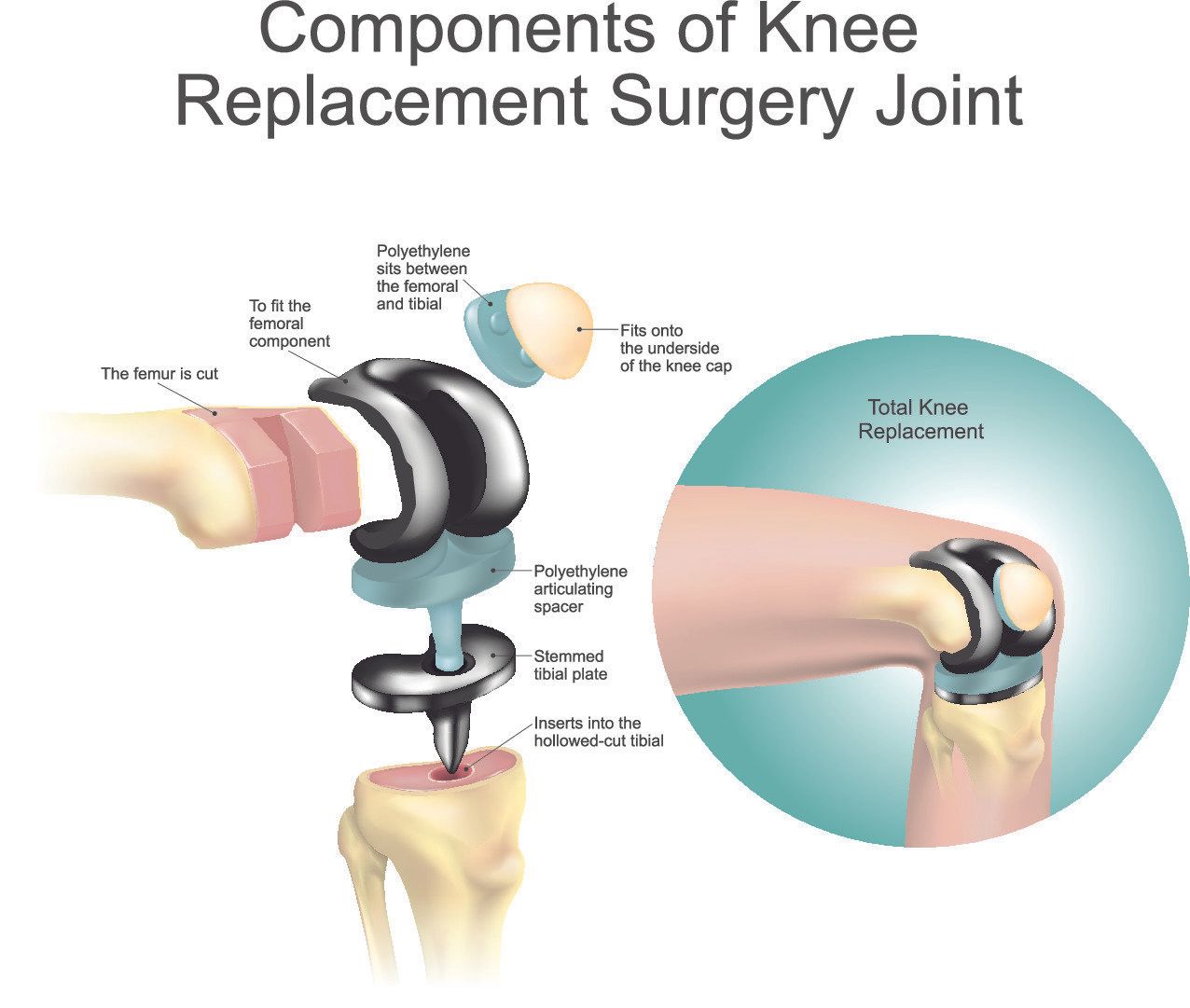
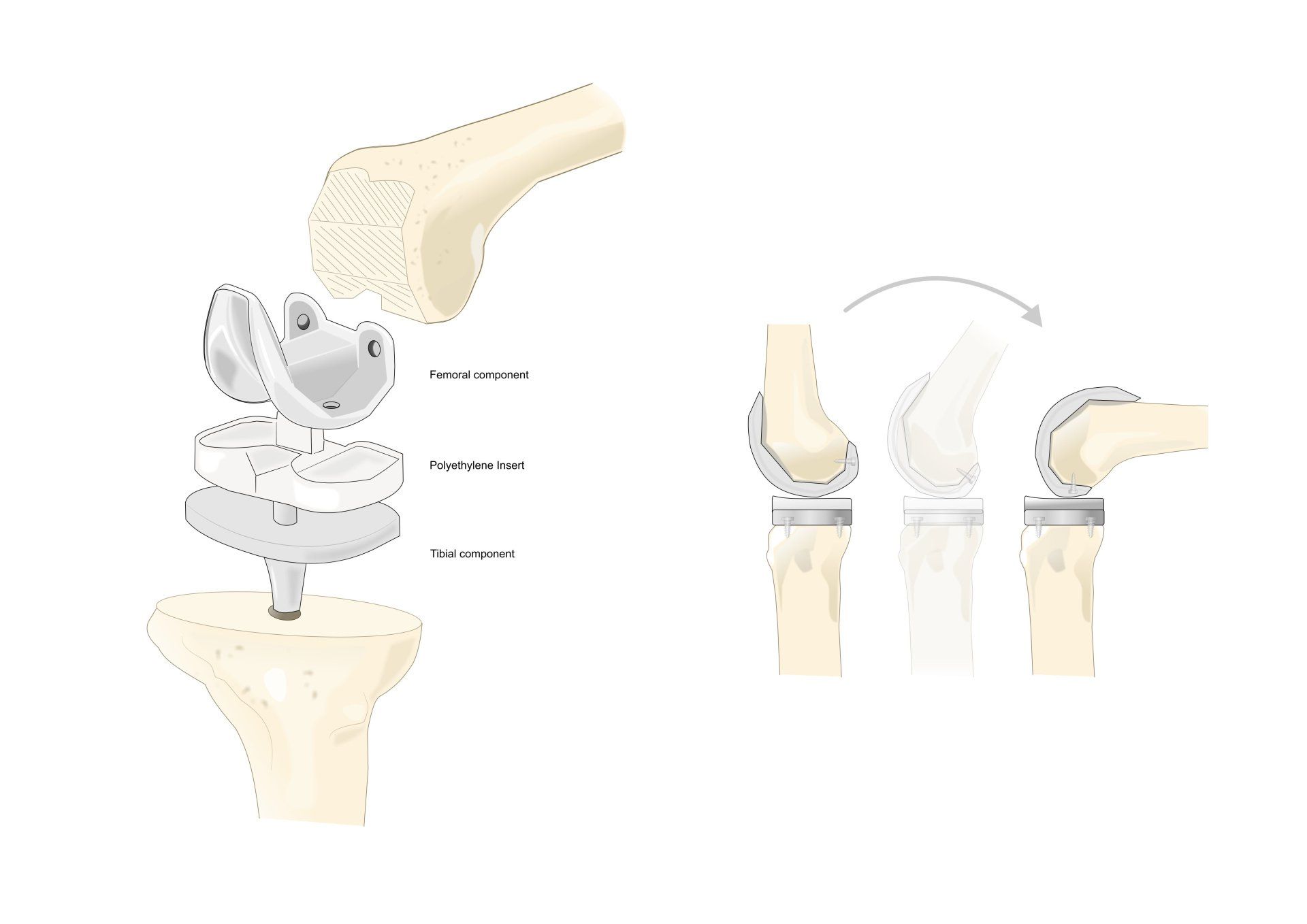
- Total knee replacement (arthroplasty) involves taking away thin layer of the arthritic (worn out) joint surface of the femur (thigh bone) and tibia (shin bone) and replacing it with metal which is secured in place with special medical grade bone cement
- In between the two metal surfaces a plastic insert is placed (polyethylene)
- In selected cases (pending on the degree of wear and pain at the front of the knee) the back end of the patella (kneecap) may also be resurfaced with polyethylene which is cemented in place
Investigations
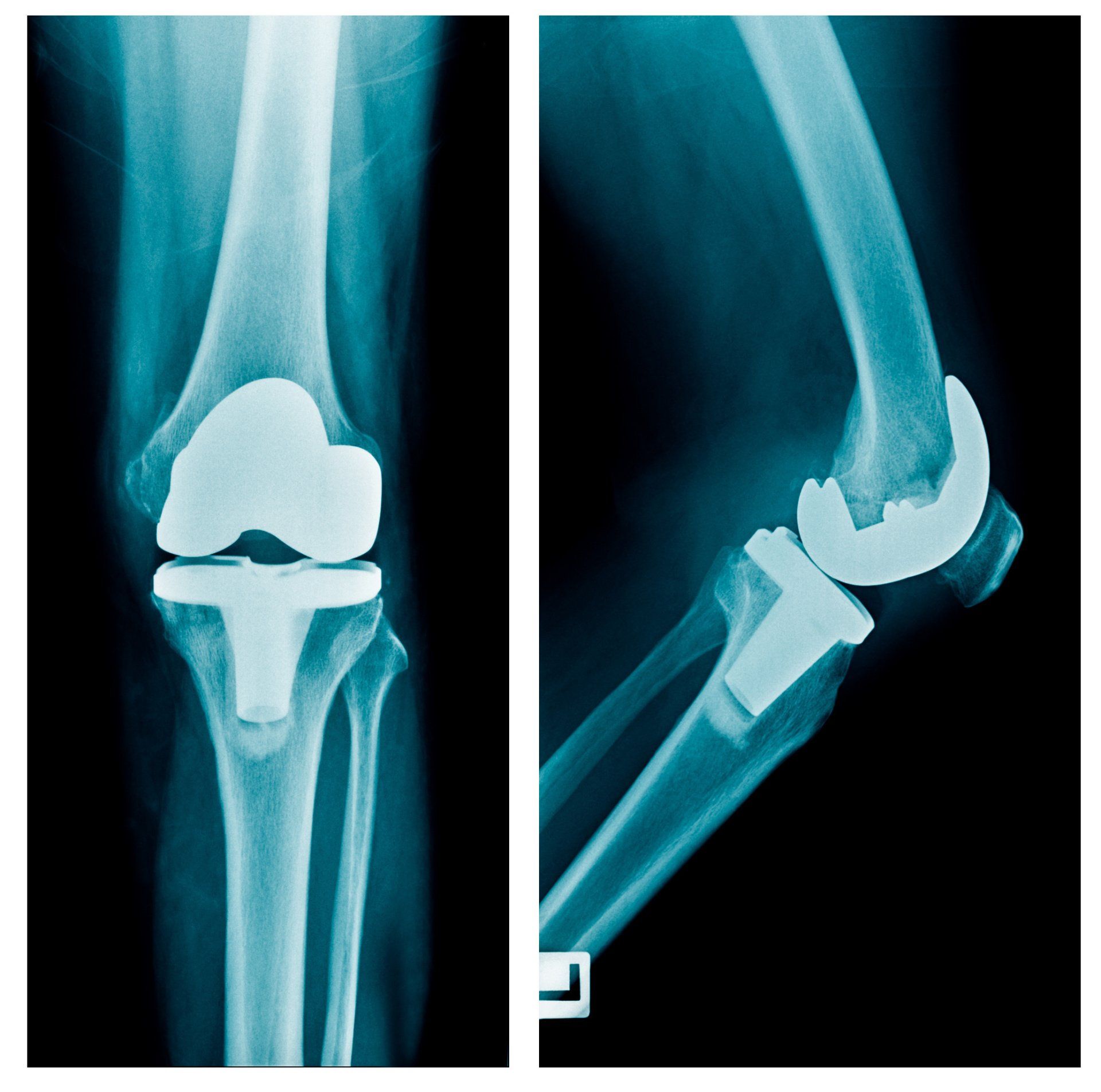
- X-rays
- AP (frontal view): helps confirm that the inner and outer knee compartments are not affected by marked arthritis
- Lateral (side view): assess degree of wear in patellofemoral compartment
- Skyline view: helps show degree of wear between patella and femur
Indications
- Severe and widespread arthritis in the knee
- Severe knee pain that limits activities of daily living:
- Walking
- Getting up from a chair
- Going up and down stairs
- Pain at rest
- Pain that wakes you up at night
- Pain not relieved adequately with painkillers and other conservative options
Expectations
- About 90% of patients following TKR report excellent results with significant improvement in function and loss of pain
- 5% are about the same following a TKR and 5% are worse off
- About 95% of TKRs are working fine after 10 years
- About 80% of TKRs are working fine after 20 years
- The younger and more physically demanding patients will wear out and loosen their implant sooner than the above data which have been widely reported in the elderly population
Risks and Complications
- Despite 90% of patients having excellent results unfortunately as with any major operation there are potential risks and complications for a total knee replacement:
- Pain
- Stiffness and swelling
- Blood clots
- Infection
- Nerve injury such as numbness around the scar site
- Ligament injury
- Loosening and requirement for revision
- Anaesthetic risks
Minimising Potential Risks from Occurring
- Minimise swelling and stiffness:
- Perform physiotherapy exercises as instructed
- Focus on getting the leg fully straight from day one:
- Patients often find having knee bent slightly is more comfortable than getting it fully straight but it is imperative to push the knee straight and then bend it
- The ability to get knee fully straight can be easily and quickly lost if it is avoided which has a negative impact on standing, walking and risk of ongoing pain and wear
- Minimise swelling by elevating leg first two weeks whenever you are resting:
- Elevation should be with foot vertically higher than knee which is vertically higher than hip
- This will aid getting fluid away from the lower limb through gravity
- Regular icing first two weeks or as long as swelling is present:
- Have two bags of pees (or similar cold compress) in freezer to interchange between the two
- Wrap the ice in tea towel or pillow case/thin cloth
- Do not apply ice directly to skin as can cause skin burn
- Apply for 20 minutes at a time at least 4 times a day
- Minimising swelling will help minimising risk of stiffness and reduce pain
- Specifically designed medical devices exist that help apply circumferential cold therapy and intermittent compression:
- They provide more effective cold and compression than ice packs and so expedite rehabilitation
- However, there is an additional cost involved
- Blood clot prevention:
- Drink plenty of fluids, particularly water
- Carry out regular exercises as shown by physiotherapy
- Take your blood thinning medication as instructed
- Wear your thromboembolic deterrent stockings as instructed
- Seek prompt medical help if:
- Blood clot in leg has developed (Deep Vein Thrombosis):
- Increasing pain in calf
- Tender or redness above or below your knee
- Increasing swelling in calf, ankle, foot
- Blood clot has travelled to your lung (Pulmonary Embolus):
- Sudden and increasing shortness of breath
- Sudden onset sharp chest pain that may be worse with deep breathing or coughing
- Rapid heart rate
- Coughing up blood
- Sweating
- Anxiety
- Preventing Infection:
- Unfortunately infections elsewhere in the body can travel round the blood stream and settle around the knee
- Superficial infections (i.e. close to the skin) can often be easily treated with a course of antibiotics
- Deeper infections involve bacteria sticking onto the metal implant and can form a membrane around themselves that protects them from antibiotics reaching them:
- To effectively treat the deep infection, it often requires removal of implants, and putting a temporary cement spacer which fills the void and provides a locally high antibiotic concentration to helps eradicate the infection
- Once 6-12 weeks have passed and if markers of infection are back to normal then a second operation is carried out to put a definitive knee replacement in
- This is why a deep infection is a serious complication and every effort is made to minimise this risk
- It is therefore imperative that any wounds and infections elsewhere in the body are treated promptly
- Warning signs for possible knee replacement infection:
- Increasing pain in the knee both at rest and in particular movement
- Increasing warmth, redness, swelling of knee and its wound
- Wound leaking fluid especially pus
- Spiking temperatures (more then 38 degrees Centigrade)
- Sweating
- If there is suspicion for infection please contact your surgeon immediately
- Avoiding falls and periprosthetic fractures:
- This occurs when the bones around the knee replacement break following a fall often necessitating in complex surgery
- It is therefore important the first few weeks to use walking aids (cane, crutch, walker, someone else assisting) until balance, strength and flexibility are regained and can safely walk independently
- Guidance for this will be provided by your surgeon and physiotherapist
World Class Medical Consultation
Dr Theodorides has a logbook of over 6000 operations and a special interest in sports knee injuries, ligament reconstructions, complex meniscal repair and meniscal transplants, chondral regeneration and transplantation, anterior knee pain, patella instability, trochleoplasties, and knee arthroplasty.
CONTACT USBook an Appointment
To book an appointment with Dr Theodorides please call +30 694 0869 069,
email info@theodorideskneesurgeon.com
or fill in the form below.
Contact Us
Thank you for contacting us.
We will get back to you as soon as possible.
We will get back to you as soon as possible.
Oops, there was an error sending your message.
Please try again later.
Please try again later.
Dr Theodorides is a UK trained Consultant Trauma and Orthopaedics knee surgeon with special interest in sports knee injuries
Request a Consultation
MENU
GET IN TOUCH
Telephone: +30 694 0869 069
info@theodorideskneesurgeon.com
Dr Anthony A TheodoridesAthens Medical Centre58 Kifisias Avenue15125 Marousi, AthensGreece
Contact us
for more information
NEWSLETTER
Join our newsletter and find out more
Contact Us
Thank you for contacting us.
We will get back to you as soon as possible
We will get back to you as soon as possible
Oops, there was an error sending your message.
Please try again later
Please try again later
Copyright © Dr Anthony A Theodorides 2020
Dr Anthony A Theodorides
MBBS, BSc, MRCS, MSc, CCT(UK), FRCS(Tr&Orth)
Consultant Trauma & Orthopaedics Knee Surgeon Specialising in Sports Knee Injuries, UK trained