Posterior Cruciate Ligament (PCL) Injury
What is the Posterior Cruciate Ligament (PCL)?
- The Posterior Cruciate Ligament (PCL) is the strongest ligament in the knee
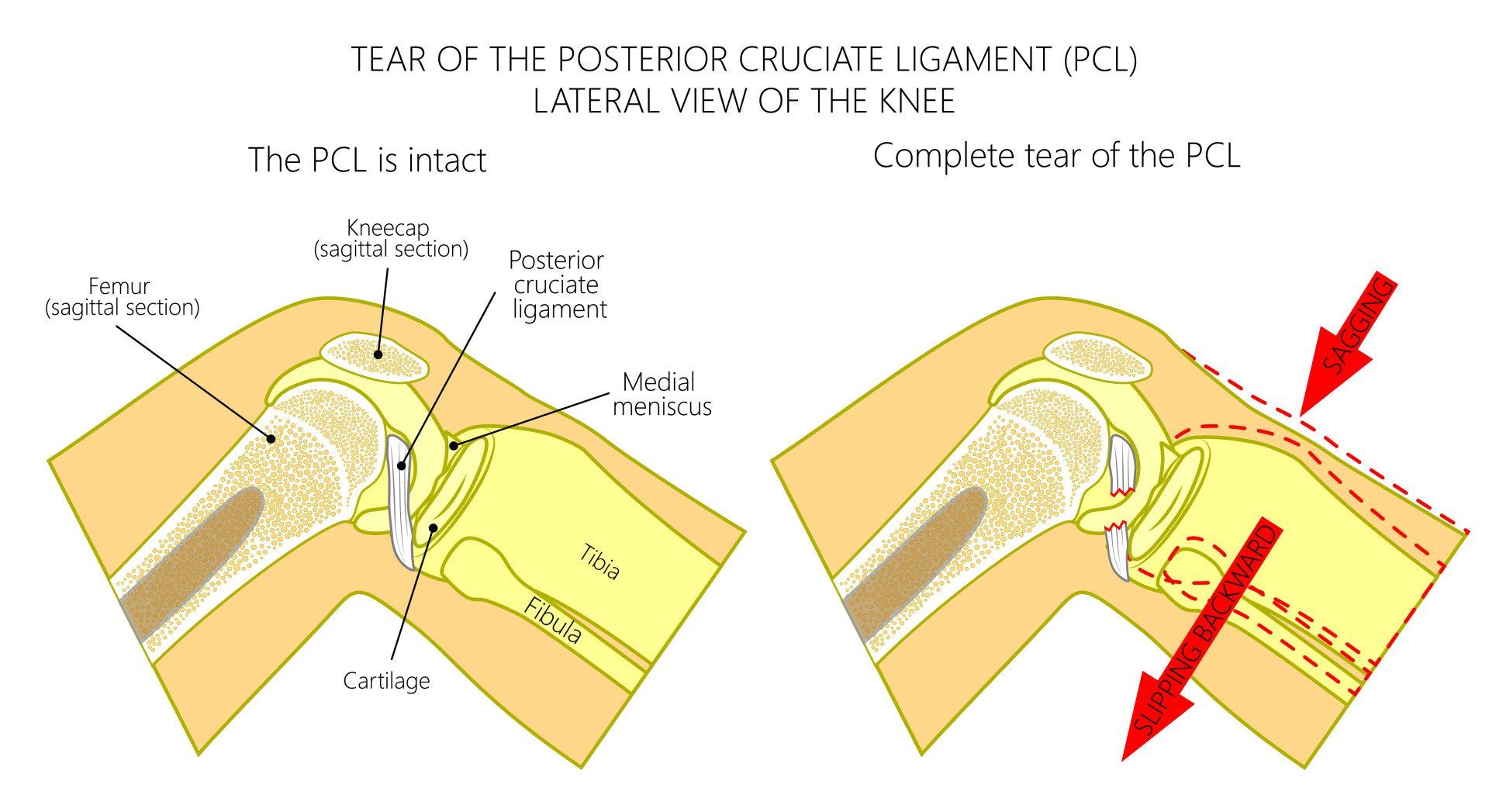
- The PCL extends from the posterior (backend) part of the central upper tibia to the medial (inner) femoral condyle
- The main function of the PCL is to prevent the tibia moving backwards (posterior) in relation to the femur
- The PCL is a secondary stabiliser to internal and external rotation of the tibia in relation to the femur
- The PCL is not commonly injured
- PCL injuries make up less than 20% of all knee injuries
- PCL injury is thought to affect 2 per 100,000 people every year
- In comparison an ACL injury affects 1 in 3,500 people every year
What is the size of the PCL?
- The PCL is 11-13 mm in diameter
- The PCL is 35-38 mm in length
Why is the PCL injured far less commonly than the ACL?
- The PCL is much stronger than the ACL
- The reason for this is due to:
- The diameter of the PCL is 1.5 times bigger than the ACL meaning that the ligament itself is much harder to break
- The area of bone that the PCL attaches is three times larger than that of the ACL:
- This means that the PCL attaches much stronger to the tibia and femur than the ACL so it is harder to tear off from these points of attachment
- PCL injury is most commonly caused by a direct blow on the tibia pushing it in a backwards direction in relation to the femur whilst the knee is flexed (bent):
- Dashboard injury:
- This occurs when the tibia hits the dashboard during a road traffic collision
- Fall:
- Landing hard directly onto the tibia with the knee bent
- These mechanisms of injury essentially overstretch and break the PCL by driving the tibia excessively posterior (backward) in relation to the femur
- PCL injuries can also happen with hyperextension or hyperflexion injury but these are less common
- Therefore unlike the ACL where the principle mechanism of injury is non-contact, the PCL is more commonly injured by a large direct blow to the knee (that pushes the tibia backwards)
- Isolated PCL injuries are rare
- >90% of all PCL injuries are associated with other ligament injuries in the knee:
- Posterolateral corner injury
- Multiligament injury
- Knee dislocation
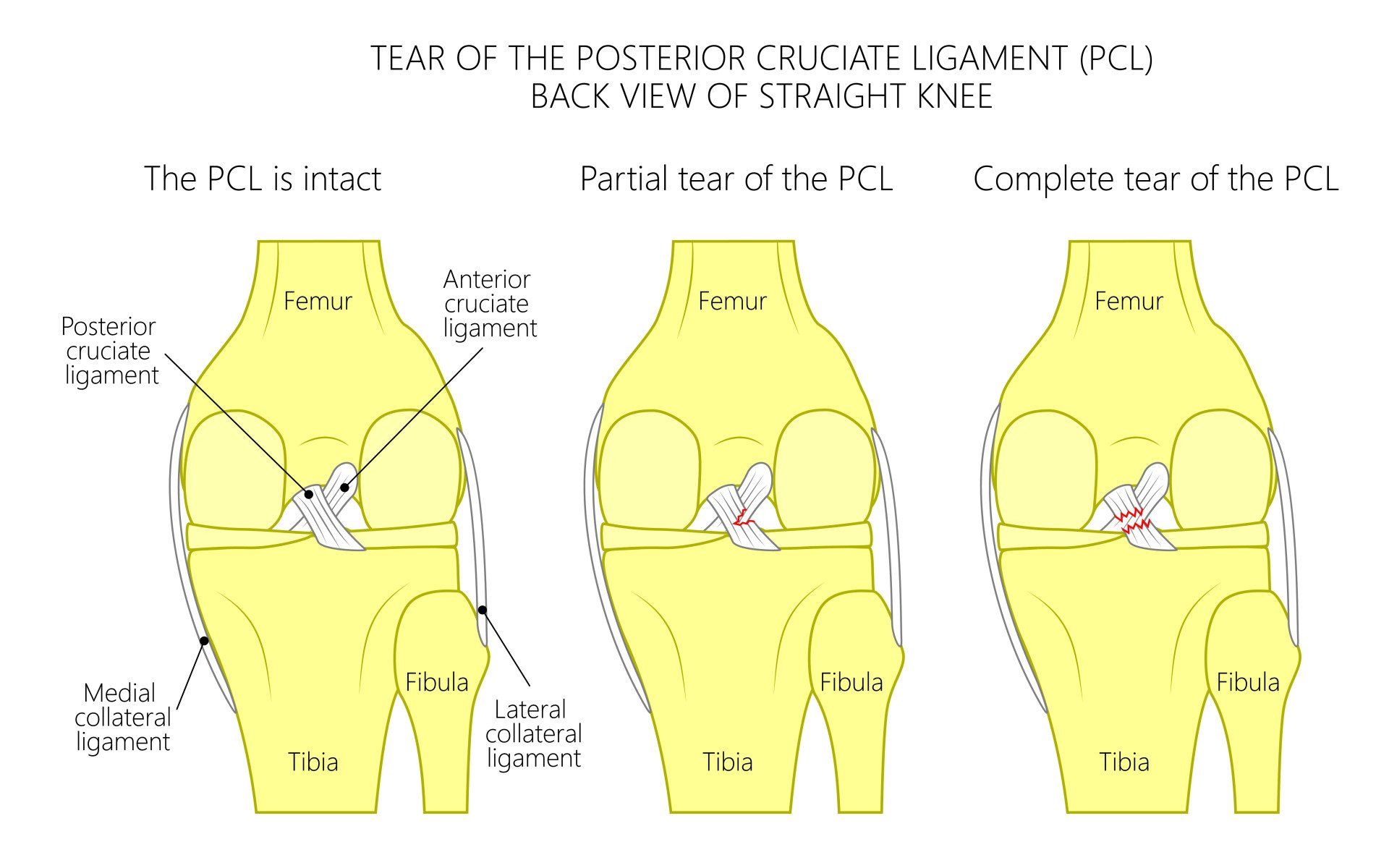
Classification of PCL injury
- This is based on the amount of posterior translation of the tibia relative to the femoral condyles with the knee bent at 90 degrees:
- Grade I: 1-5mm (mild sprain)
- Grade II: 6-10mm (moderate sprain; usually more than 50% torn):
- Grade III: >10mm (complete tear and highest risk of other ligamentous injury)
Symptoms of acute PCL injury
- The symptoms are less marked than with an ACL injury
- This means that patients often present many months later
- Pain and tenderness often quite vague and deep within the knee, but sometimes felt towards the back
- Pain is less marked than an ACL and patient can often walk off the field of play unlike ACL injuries when normally they require assistance
- Tearing can be felt but there is no pop like an ACL tear
- Swelling:
- Knee swelling following a PCL rear is much less than an ACL tear
- Stiffness
- Symptoms will depend on severity of PCL injury:
- Grade I:
- knee will feel stable
- Some pain and discomfort towards the back of the knee
- Grade II:
- PCL will be loose but not commonly associated with instability
- If knee does feel unstable often associated with another ligament injury
- Grade III:
- Commonly associated with other ligament injuries such as lateral collateral ligament (LCL) and posterolateral corner (PLC)
- Knee feels unstable
- Difficulty going downstairs and downhills
Why do PCL injuries tend to present late (i.e a long time after the initial injury)?
- PCL injuries often present late because:
- They are overall not as symptomatic as other ligamentous injuries
- They cause less acute pain, less knee swelling and less rotational instability than an ACL tear
- As a result of PCL injuries being less symptomatic in the acute phase they tend to be found coincidentally when the patient presents with symptoms consequent to a chronic PCL tears
- The consequences of chronic PCL injuries are:
- Increased back and forth sliding of the tibia in relation to the femur
- Increased risk of medial (inner) meniscal tears
- Increased risk of arthritis in the medial (inner) part of the knee:
- At 5 years following a PCL tear 80% of patients will have medial knee arthritis
- Increased risk of arthritis behind the patella (kneecap):
- At 5 years following a PCL tear 50% of patients will have arthritis behind their patella
- Chronic PCL injuries present with:
- Pain at the medial (inner) part of their knee due to medial meniscal tear and medial arthritis
- Pain at the front of the knee due to arthritis behind the patella
- Pain going down stairs and down slopes due to arthritis behind the patella
- Pain and instability on turning, twisting and pivoting
- Pain and instability with decelerating movements
How is a PCL injury diagnosed?
- PCL injury is suggestive from the history of the injury and the examination findings
- X-rays:
- Required to exclude fractures
- Stress radiographs are very helpful:
- These are X-rays taken with pressure on the tibia to push it backward which can then be detected on X-rays and therefore demonstrate the clinical insufficiency of the PCL to prevent this movement
- MRI scan:
- Helps to diagnose PCL injury
- Helps exclude other knee pathology which most often exist such as other ligament, meniscal and cartilage injuries
What is the treatment of a PCL Injury?
- Most isolated Grade I PCL sprains do well with appropriate conservative management:
- Special knee brace must be applied promptly that helps bring the tibia forwards to the neutral position in relation to the femur
- This helps position the tibia in the optimal position for the PCL to heal
- Without the brace the tibia sits too far backwards and the knee will remain slack and unstable
- Extensive physiotherapy rehabilitation focusing mainly on quadriceps strength
- Most Grade III (complete) tears require prompt PCL reconstruction
- There is increasing evidence that Grade II PCL injuries especially those that have symptomatic instability should be surgically treated in order to avoid early knee degeneration
- Bracing of knees with chronic PCL injuries will not aid or improve PCL healing but can provide symptomatic relief
- The presence of other ligament injuries in addition to the PCL tear then surgery tends to be the recommended option
- If at the time of PCL reconstruction other ligament injuries are not addressed then there is high risk of failure
What is the prognosis following a PCL tear?
- Most people do well following a PCL injury if managed correctly
- Chronic PCL deficient knee poses increased risk for:
- 75% chance of developing cartilage degeneration within 5 years to medial femoral condyle
- 50% chance of developing cartilage degeneration within 5 years to patella
How does a PCL tear differ to an ACL tear?
- The PCL is injured typically when there is a strong impact on the tibia pushing it backwards such as falling directly onto the knee or hitting the tibia on the dashboard whereas the ACL is torn by a non-contact twisting knee injury
- PCL tears are most commonly partial tears whereas ACL tears tend to be complete tears
- When the PCL is injured the pain and swelling is not as severe as when the ACL is injured
- That is why many PCL injuries present late once secondary damage have occurred and become symptomatic such as meniscal and cartilage degenerative changes
- On the other hand since ACL tears tend to be complete and present straight away with instability patients seek early medical consultation
- The PCL is much thicker and therefore much stronger than the ACL requiring a lot more force to injure it
- A far greater proportion of PCL injuries can be managed non-surgically in a suitable knee brace and intensive physiotherapy whereas most ACL tears will need reconstruction