Knee Realignment Osteotomies
Further information on lower limb malalignment, the causes and explanation of the various types such as varus and valgus knees can be found here
Overview
- Realignment osteotomy is a procedure that involves intentionally breaking a bone, realigning it and fixing it in place with hardware (typically a metal plate and screws)
- It is carried out because the angle the femur (thigh bone) and tibia (shin bone) make around the knee is abnormal and/or the wear of the cartilage on one side of the knee is severe enough to concentrate the weight bearing forces on the worn-out part of the knee
- By realigning the lower limb the weight bearing forces are shifted away from the arthritic and painful part of the knee and so providing pain relief
- A knee osteotomy is considered for patients who have painful arthritis in their knee but are too young for a joint replacement
- Knee osteotomies do not involve making a cut to the joint surface which is left in tact:
- Unlike a joint replacement the arthritic portion of the knee joint in the osteotomy is not changed
- Pain relief is obtained by simply offloading the forced from the arthritic part
For which patients is knee osteotomy suitable?
- Young active patient <60 years
- Osteoarthritis and pain affecting only one side of the knee
- Healthy individuals with good blood circulation in their legs
- Non-obese patients
For which patients is knee osteotomy not suitable?
- Inflammatory arthritis such as rheumatoid arthritis
- Arthritis affecting both sides of the knee
- If unable to get knee fully straight and bend it beyond 90 degrees
- Presence of gross ligament instability
- Smoking:
- This has been shown to increase risk of the osteotomy not uniting
- For bone healing to occur there needs to be good microcirculation
- Smoking adversely affects microcirculation in tissues including bone
- This results in higher risk of delayed bone healing in smokers and even non-union whereby the fracture does not unite at all and requires further complex surgery to kickstart the healing process
- An osteotomy is an intentional and precise fracture (break in the bone) and it will be affected by smoking much like any fracture secondary to trauma
- Whilst stopping smoking at least 2 weeks before the operation can help, it would be insufficient in chronic heavy smokers when the damage to microcirculation is too severe
Benefits of an osteotomy and biological knee preservation
- It preserves the life span of the natural knee joint by correcting poor knee alignment
- Osteotomy is one of the key operations in biological knee preservation as it restores joint biomechanics which is vital for the longevity of any knee
- Improves pain by shifting the forces away from the worn out painful part of the knee
- Delays the need for a joint replacement operation typically for 10-15 years
- Better range of motion than a joint replacement
- Patients can be more active following an osteotomy than following a joint replacement:
- Patients following knee arthroplasty will be able to mobilise full weight bearing sooner than with an osteotomy but once the osteotomy site fully heals it allows patients to perform full impact activities
- Patients with a joint replacement are advised not to do high impact activities as this increases the stresses on and around the implant which then expedites the wear and tear of the implant and can loosen it from the bone which would lead to a premature revision operation
- More suitable for young active patients and those in physically demanding jobs such as in construction, plumbers, and farmers
Disadvantages of an osteotomy
- Rehabilitation is longer than a joint replacement
- Unlike a joint replacement walking full weight bearing on the operated leg is delayed with an osteotomy so as to give time for the bone to heal without displacing the osteotomy
- Pain relief is slightly less predictable
- Slightly more complications than a joint replacement
Is timing important for an osteotomy?
- The purpose of an osteotomy is to shift the forces away from the damaged and painful part of the knee
- The articular cartilage on the other side of the knee needs to be preserved
- If the knee degeneration is left for a long time then the arthritis will spread to the other side of the knee and in this scenario an osteotomy is not advisable:
- In order for the osteotomy to be successful the other side of the knee needs to be well preserved in order to tolerate the increased forced going through it without causing pain
- When the arthritis is more widespread the patient is heading towards a knee replacement
Investigations
- X-rays of the knee:
- Shows degree and location of wear inside the knee and deformity around the knee
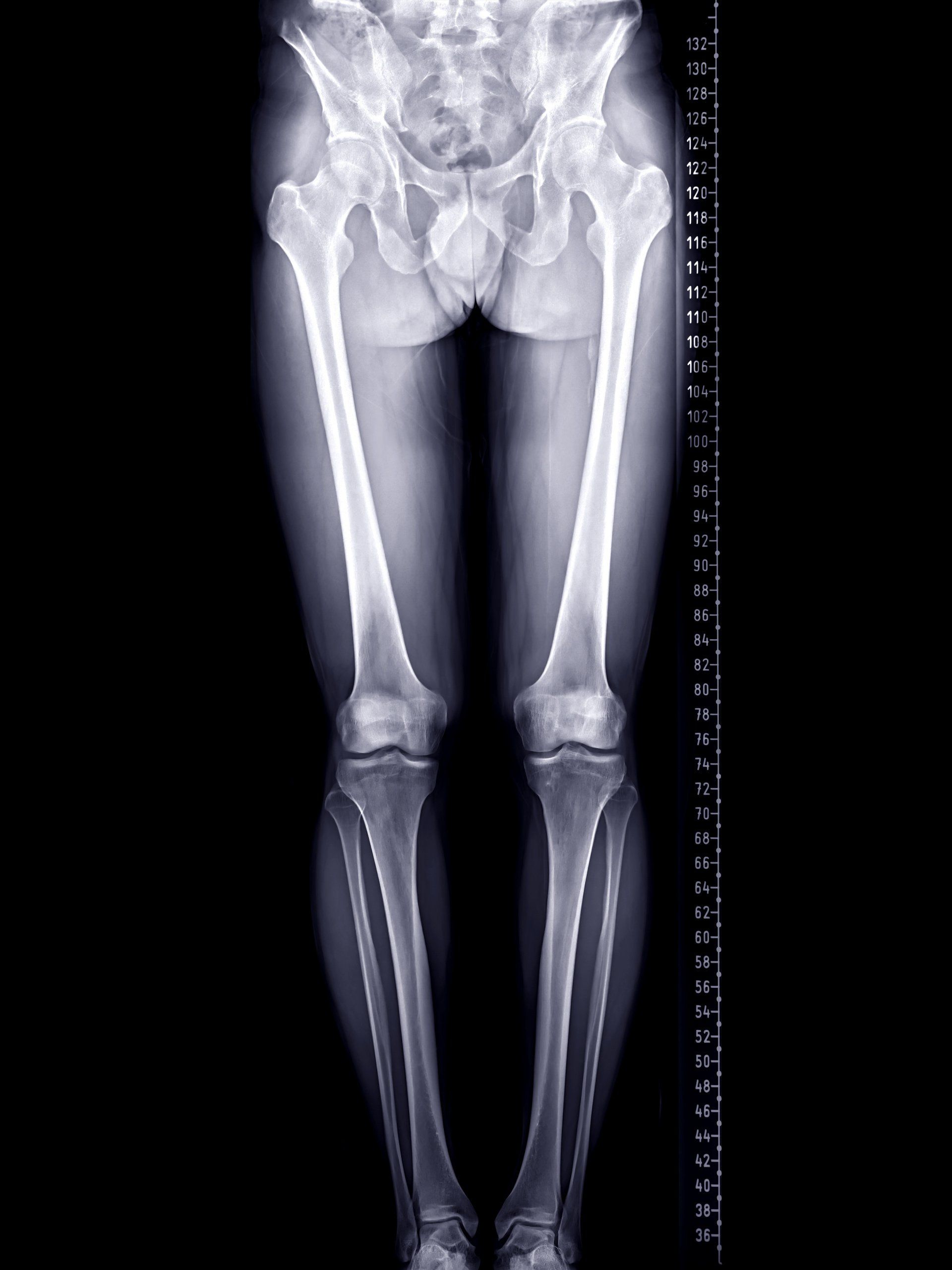
- Long leg alignment views:
- X-rays taken of both lower limbs whilst standing and cover from pelvis to feet
- MRI scan of the knee:
- Shows degree and location of cartilage wear around the knee
- Importantly it shows degree of wear in the non-painful side which will determine whether osteotomy is suitable
- Will also show injury to ligaments and menisci which may need addressing
- From the long leg alignment views, the surgeon will be able to calculate the location and degree of deformity, and the amount of correction that is required
- This will then help determine:
- Where to perform the osteotomy (tibia or femur)
- Which type of osteotomy to perform (open or closed wedge)
What are the different types of osteotomies?
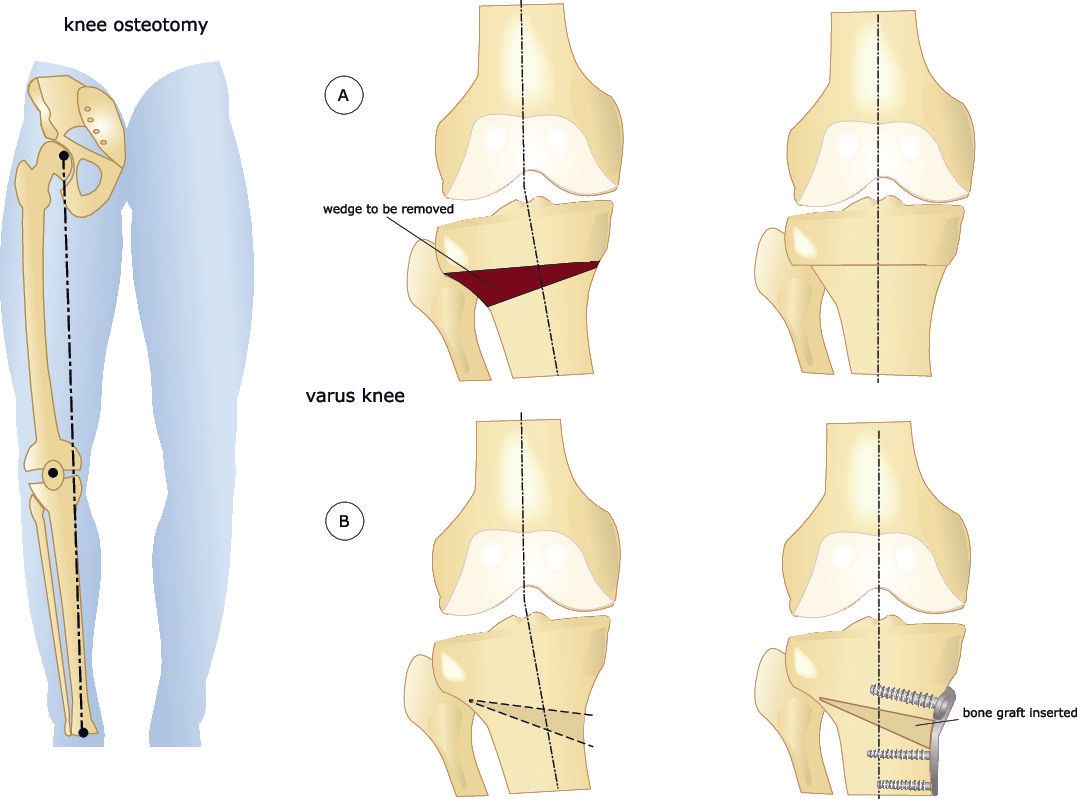
- High Tibial Osteotomy (HTO):
- This involves cutting the tibia (shin bone) close to the knee but not affecting the knee joint surface
- Realigning the tibia and holding it in place with metalwork
- This is most commonly performed for varus knees
- It can also be carried out for mildly valgus knees
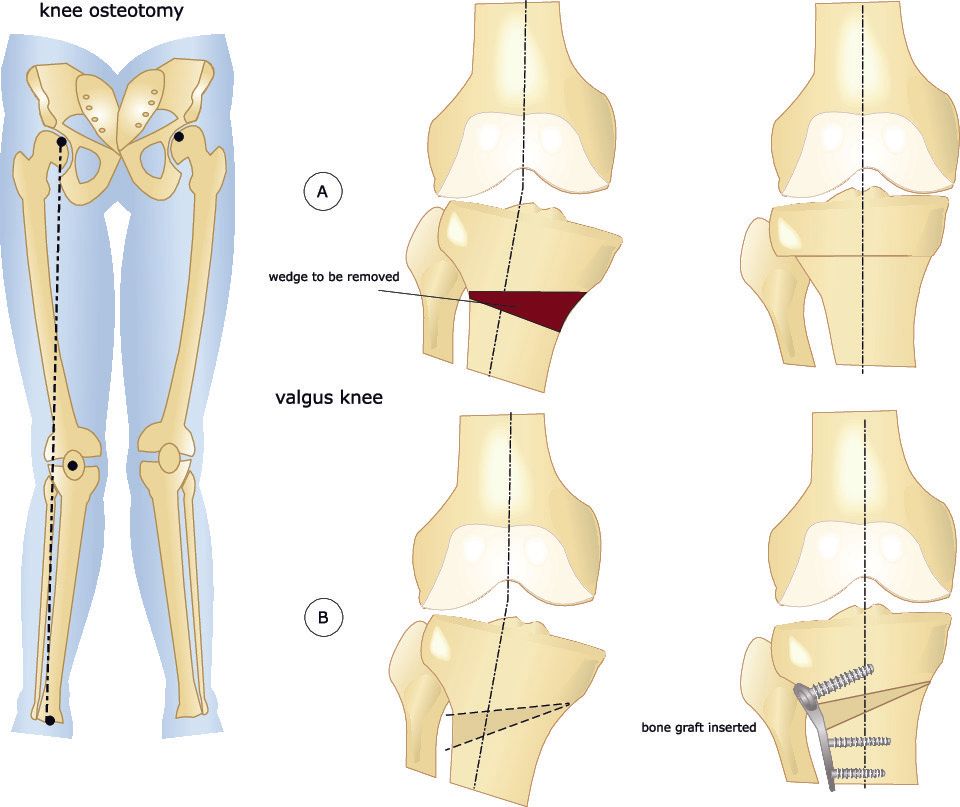
- Distal Femoral Osteotomy (DFO):
- This involves cutting the femur (thigh bone) close to the knee but not affecting the knee joint surface
- Realigning the femur and holding it in place with metalwork
- This is most commonly performed for valgus knees
- Both the high tibial and the distal femoral osteotomies can be performed:
- Opening wedge:
- This involves making a single cut in the bone and opening up the gap
- Closing wedge:
- This involves making two cuts to the bone that converge together in order to remove a wedge of bone
- The gap is then closed by bending the bone at the small
- On the medial (inner) or lateral (outer) side of either the tibia or femur:
- They each have their own advantages and disadvantages
- To correct a deformity the osteotomy can be performed on either side of the same bone but on one side it will be opening wedge and on the other a lateral wedge
- A varus knee deformity can be corrected with a medial opening wedge osteotomy (more common) or a lateral closing wedge osteotomy of the proximal (upper) tibia
- A valgus knee deformity can be corrected with a medial closing wedge osteotomy (more common) or a lateral opening wedge osteotomy of the proximal (upper) tibia
Osteotomies can also be carried out for knee instability
- There are various types of knee instability that are due to abnormal joint biomechanics that can be improved with an osteotomy
- Tibial slope changing osteotomy:
- When looking at the tibia from the side there is normally a small downhill slope going from front to back
- Sometimes this downslope is excessive and the result is when standing the femur slides backwards in relation to the tibia
- This is the same effect as the tibia going forwards in relation to the femur
- This places excessive stresses on the ACL and is something that is often overlooked in ACL reconstructions and put the graft at high risk of failure
- A tibial slope changing osteotomy to make the slope more horizontal will protect the ACL graft
- The contrary is true with a posterior cruciate ligament (PCL) injury
- The function of the PCL is to stop the tibia translating backwards in relation to the femur
- Sometimes the tibial slope is reversed and it’s uphill
- In this scenario the tibia will slide backwards in relation to the femur when standing so putting excess forced in the PCL
- Uphill tibial slopes may also present with a patient being able to bend their knee too far backwards
- In both these scenarios correcting the tibial slope to be down sloping will help with both pathologies
Tibial Tubercle Osteotomy (TTO)
- This is a common operation for patellofemoral instability and is discussed further in that section
What does a knee osteotomy involve?
- Following evaluation of preoperative investigations, the surgeon would calculate the degree of deformity and its location and planned whether to perform a high tibial osteotomy or a distal femoral osteotomy and in rare occasions both
- Before proceeding with the osteotomy, a knee arthroscopy is carried out:
- This helps evaluate the amount of cartilage wear throughout the knee especially how severe it is on the painful side and to ensure there is minimal wear on the other side
- Menisci are assessed and if necessary treated where possible
- A skin incision is made either on the proximal medial end of the tibia or distal medial end of the femur and careful dissection down to the bone
- With the aid of a bone saw a precise cut is made under the guidance of a special X-ray machine called Image Intensifier
- The bone cut is not completed though to the other side but rather leave a small bone hinge in one corner
- In this way the bone is weakened but still in one piece allowing the surgeon to change the alignment of the bone without breaking it
- In an open wedge osteotomy a clamp is placed within the bone cut and the gap opened to the desired amount
- Depending on the size of the gap bone graft may be used to fill the gap
- This bone graft can be:
- Autograft:
- Bone graft taken from another part of the patient
- Allograft:
- Bone graft taken from a donor
- Synthetic graft:
- Artificially made bone graft
- In a closed wedge osteotomy two bone cuts are made to the bone (instead of one) so that a wedge of bone can be removed and then the bone realigned to close the gap and the bone ends to touch
- With both open and closing wedge osteotomies the osteotomy is secured with metalwork which is typically a plate and screws
- The wound is then washed and closed
Complications
- Infection:
- Risk is small at <1%
- Superficial infections that only involve the skin are treated with a course of oral antibiotics
- Deep infections despite being rare are more complicated:
- Wounds need to be washed in theatre
- If the knee joint is affected then this will also need to be washed out
- Intravenous antibiotics will be required and then can be switched to oral when the infection is more controlled
- Oral antibiotics may need to be taken until the plate can be removed after a year when the fracture has healed
- Risk of infection is higher in smokers, diabetics, obese, poor blood circulation in legs, and if patient is on immunosuppressant medications such as steroids
- Should avoid getting cuts and grazes around the knee and leg especially before the operation so as to minimise risk of bugs entering the circulation and causing an infection
- Blood clots:
- Blood clot in a calf vein is called deep vein thrombosis (DVT):
- <2% of patients get DVT
- It presents with increasing pain and swelling in the calf
- Diagnosed with an ultrasound scan of the calf
- Patients should contact their operating surgeon
- If the blood clot in the calf breaks away and lodges in the lungs it is called a pulmonary embolus (PE):
- This is extremely rare <0.2%
- It presents with shortness of breath, sharp chest pain worse on deep breathing or coughing, rapid heart rate and breathing, sweating, sometimes coughing up blood or pink stained mucus
- Diagnosed with a special CT scan of the chest
- Patients should seek immediate medical help
- Medication to thin your blood will be required for a period of time to prevent the clots getting bigger:
- The dose and duration of these medications is greater for a PE
- Swelling and pain:
- Patients experience more pain and swelling than a joint replacement
- Because the arthritic part of the joint is not directly altered as with a joint replacement but rather offloaded, there is a small risk of ongoing long-term pain
- Stiffness:
- It is important to be compliant with the rehabilitation protocol in order to prevent stiffness of the knee
- Numbness around the scar site:
- It is common to have a patch of numbness or altered sensation around a surgical scar
- Most do improve over time but not always
- Delayed or non-union of the osteotomy site:
- Delayed union means the osteotomy takes much longer than expected to heal
- Non-union means the osteotomy does not unite at all over time
- Risk of delayed and non-union in smokers is ~20% vs <5% in non-smokers
- Delayed and non-union of the osteotomy site will require optimisation of bone healing through nutrition, cessation of smoking, compliance with rehabilitation, and may even require an additional operation
- Inadvertent fracture:
- To realign the bone a special saw is used to cut the bone while leaving a small hinge of bone still intact which is used to help bend the bone a few degrees to realign it
- During this bending of the bone at the hinge it may inadvertently crack and/or a fracture propagate towards the knee joint
- These inadvertent fractures are often very small and not always picked up in theatre despite the use of an X-ray machine
- Additional surgery may be required to stabilise the additional fracture
- Nerve injury:
- There is a nerve on the outside outer part of the knee, called the common peroneal nerve
- Injury to this nerve is rare and can produce numbness between the big toe and the adjacent toe or worse can lead to foot drop which is extremely rare:
- Foot drop is the inability to pull the foot up towards you and clear the ground when you walk
- People who get this stumble over when they walk as a result, so they need to wear a special orthotic around the ankle to help them walk
- Performing a high tibial osteotomy from the medial (inner) side carries a smaller risk than performing it from the lateral (outer) side of the upper tibia and so it is the preferred approach for a tibial osteotomy
- Compartment syndrome:
- This occurs when pressure builds up in the space around the muscles to a level that reduces blood flow to them and they are starved of oxygen and nutrients
- It is an extremely painful condition with severe swelling
- It is an orthopaedic emergency and if suspected requires urgent surgical release of the pressure in theatre
- Whilst this is a rare complication <0.1% it is important to take all measures to minimise swelling and progression to compartment syndrome
- Metalwork irritation:
- The metal plate and screws which are used to hold the osteotomy can irritate the skin and/or muscles
- The metalwork can be removed once the osteotomy has fully united typically after a year
Rehabilitation after an osteotomy
- Most people are home within 2-3 days
- Wound care is important
- Controlling the swelling will be key to recovery with lots of repeated icing, resting and elevating the leg
- Mobilising feet and ankles are encouraged to aid circulation and help prevent blood clots
- As the bone is intentionally broken and then fixed in place, it takes time for the bone to heal as with any fracture
- The progress of rehabilitation and weight bearing status can be quite variable and will depend on numerous factors such as:
- In a closing wedge osteotomy, the bone ends meet so this is a more stable construct than an opening wedge osteotomy where the bone ends of the osteotomy do not meet
- The insertion of a bone wedge in an opening osteotomy can help expedite the healing and the type of bone wedge also has an impact (autograft provides quicker healing than allograft or synthetic graft)
- The type of hardware used to secure the osteotomy
- The weight of the patient, overall health and mobility before hand
- The amount of discomfort when they weight bear
- Crutches will be required for about 8 weeks to help with stability and weight bearing
- Physiotherapy exercises will need to be carried out to improve range of motion and strength around the knee
- The knee will be placed in a hinged knee brace for about 6 weeks:
- The brace provides side to side support whilst allowing the knee to bend
- Patients should make arrangements beforehand regarding transportation as they won’t be able to drive for 6-8 weeks
- Whilst most patients start to walk unaided by three months it can take 6 months or more to be fully rehabilitated and feel the benefits of the operation
- It may take a year before being able to do high impact activities such as jogging
- The focus of rehabilitation is to get the lower limb stronger, improve range of motion and improve balance
Outcomes following an osteotomy
- The outcomes will vary depending on:
- Severity and distribution of the arthritis
- Stiffness prior to the operation
- Meniscal integrity and function
- High body mass index
- Continuing with high impact activities
- At 10 years following an osteotomy about 70-80% of people are happy with their pain and function
- Looking after your knee would help delay the need for joint replacement by:
- Keeping a low body mass index
- Exercising through low impact activities
- Avoiding high impact activities
More relevant information can be found on: