All About Muscles, Tendons and Ligaments
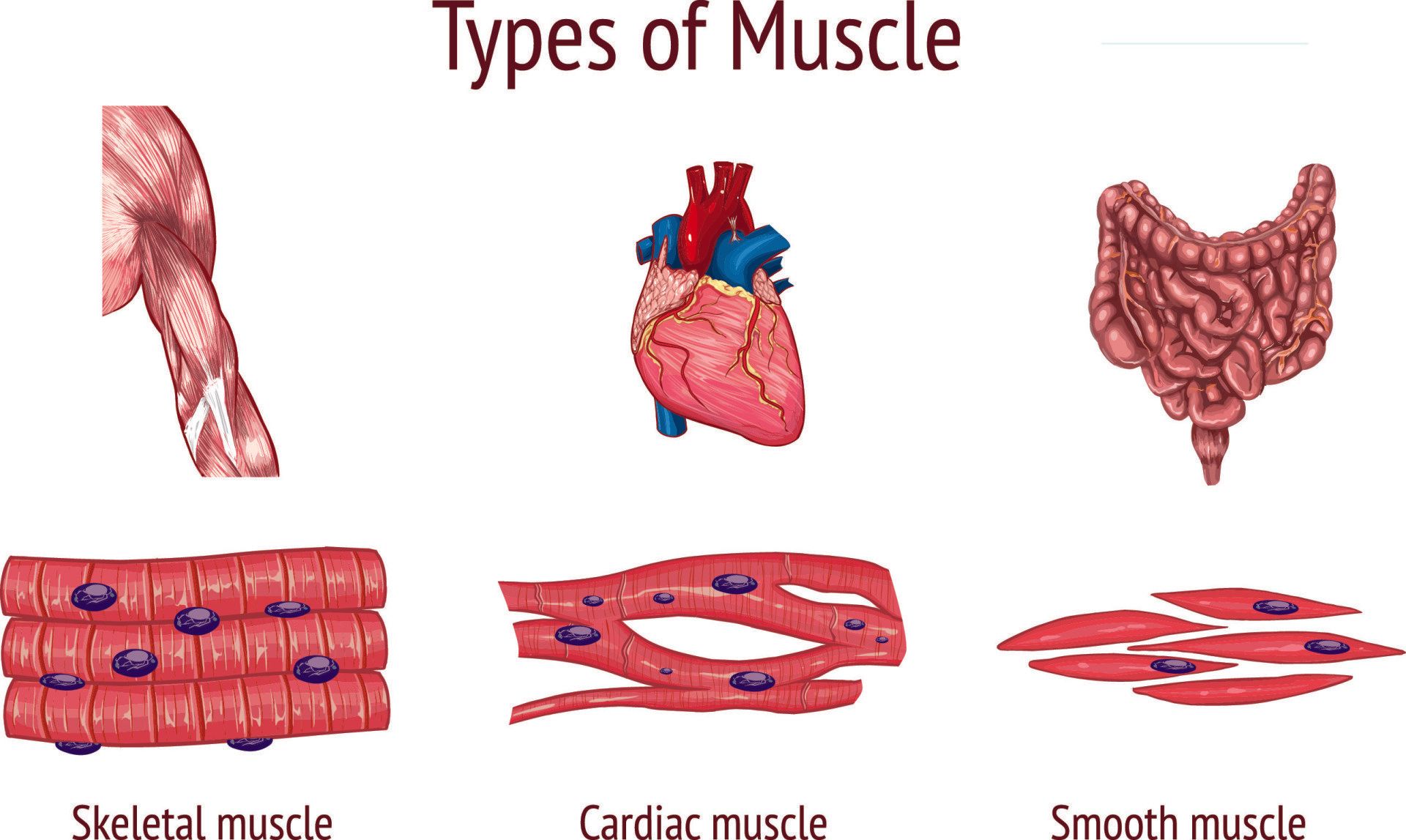
What are the different types of muscle?
- Skeletal muscle:
- This is voluntary muscle which means muscles contract on conscious demand
- They are anchored to bones via tendons and when the muscle contracts on demand it causes movement of a joint
- They are responsible for the human body to move in space and to maintain posture
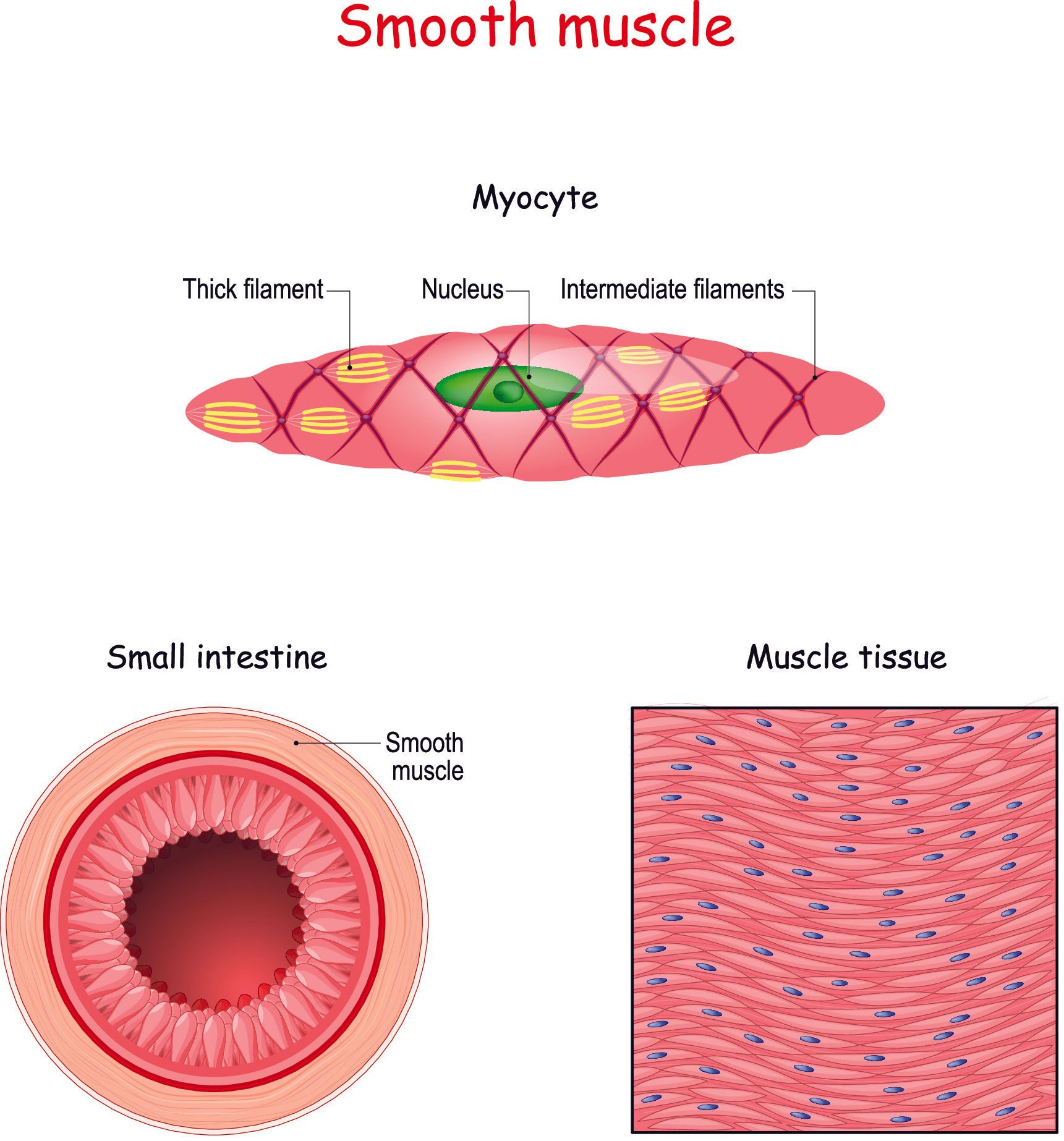
- Smooth muscle:
- This is involuntary muscle and so it is not under conscious control
- They line the walls of organs and help with vital bodily functions
- Examples of where they are located: oesophagus, stomach, intestines, bladder, bronchi in the lungs and blood vessels
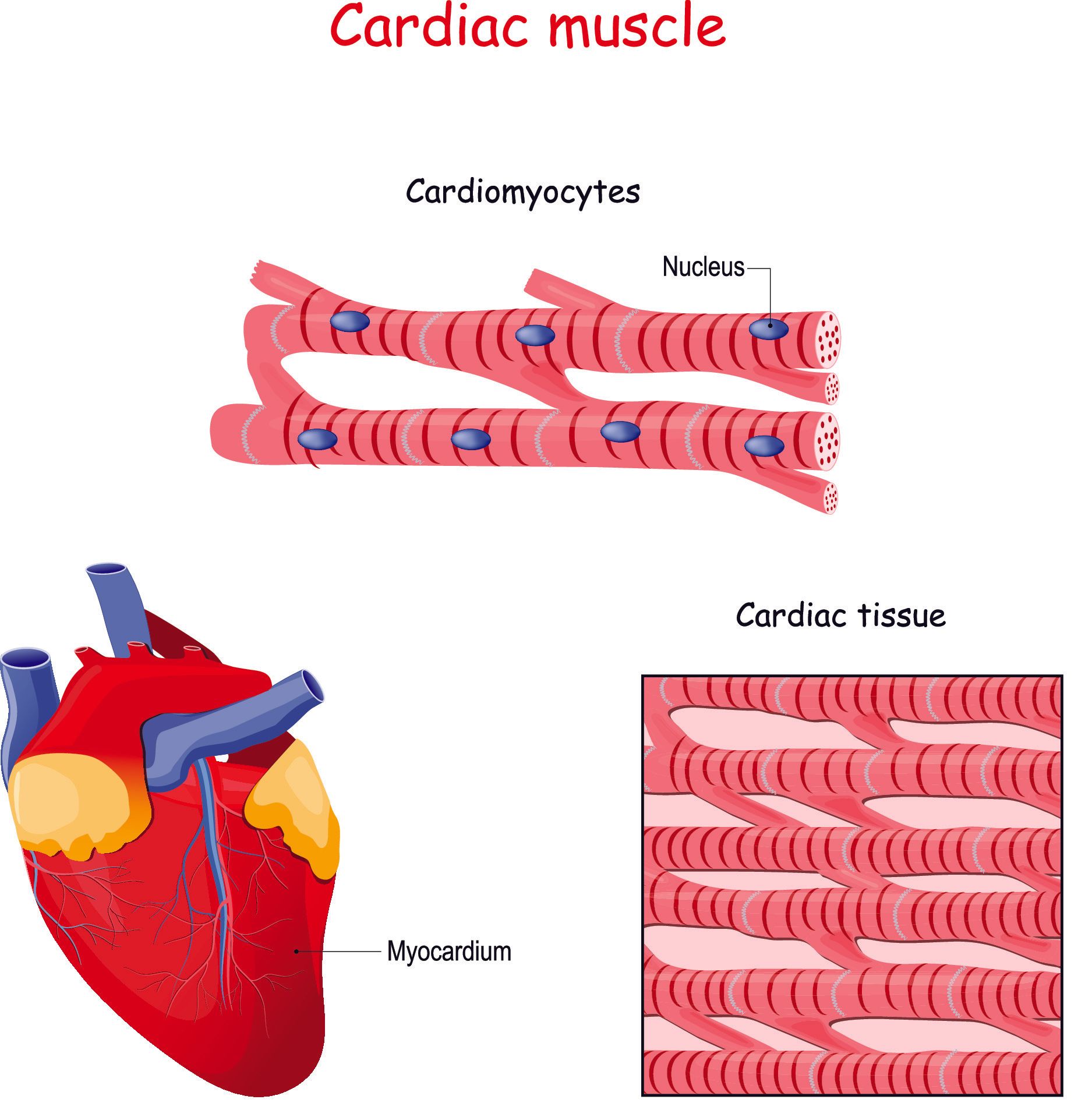
- Cardiac muscle:
- This is unique in that it is between skeletal muscle and smooth muscle
- It is involuntary like smooth muscle but its structure resembles more closely that of skeletal muscle
- It is only found in the heart
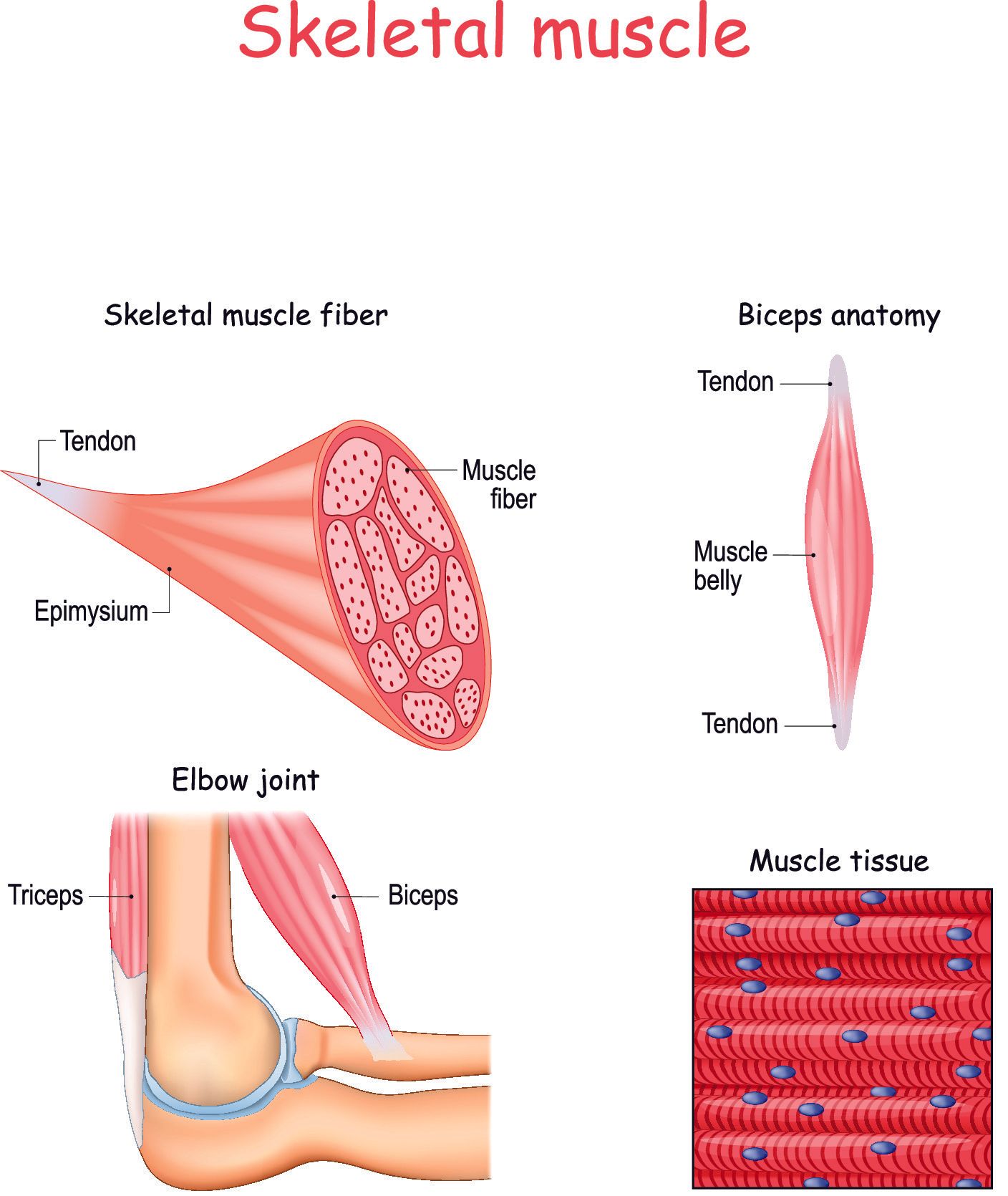
Skeletal muscle anatomy
- Whilst the number of bones in the human body is consistent at 206 the number of different skeletal muscles vary:
- There are over 650 named skeletal muscles
- Skeletal muscle is a highly organised structure with its own nerve and blood supply and connective tissue
- Skeletal muscle can vary in size and shape:
- The gluteus maximus is the largest muscle in the body and forms the largest part of the buttocks
- Has an average weight of 850g, is ~2cm thick and covers an area of ~66cm2
- Stapedius is the smallest muscle in the body and helps stabilise the stapes in the middle ear which is the smallest bone in the body
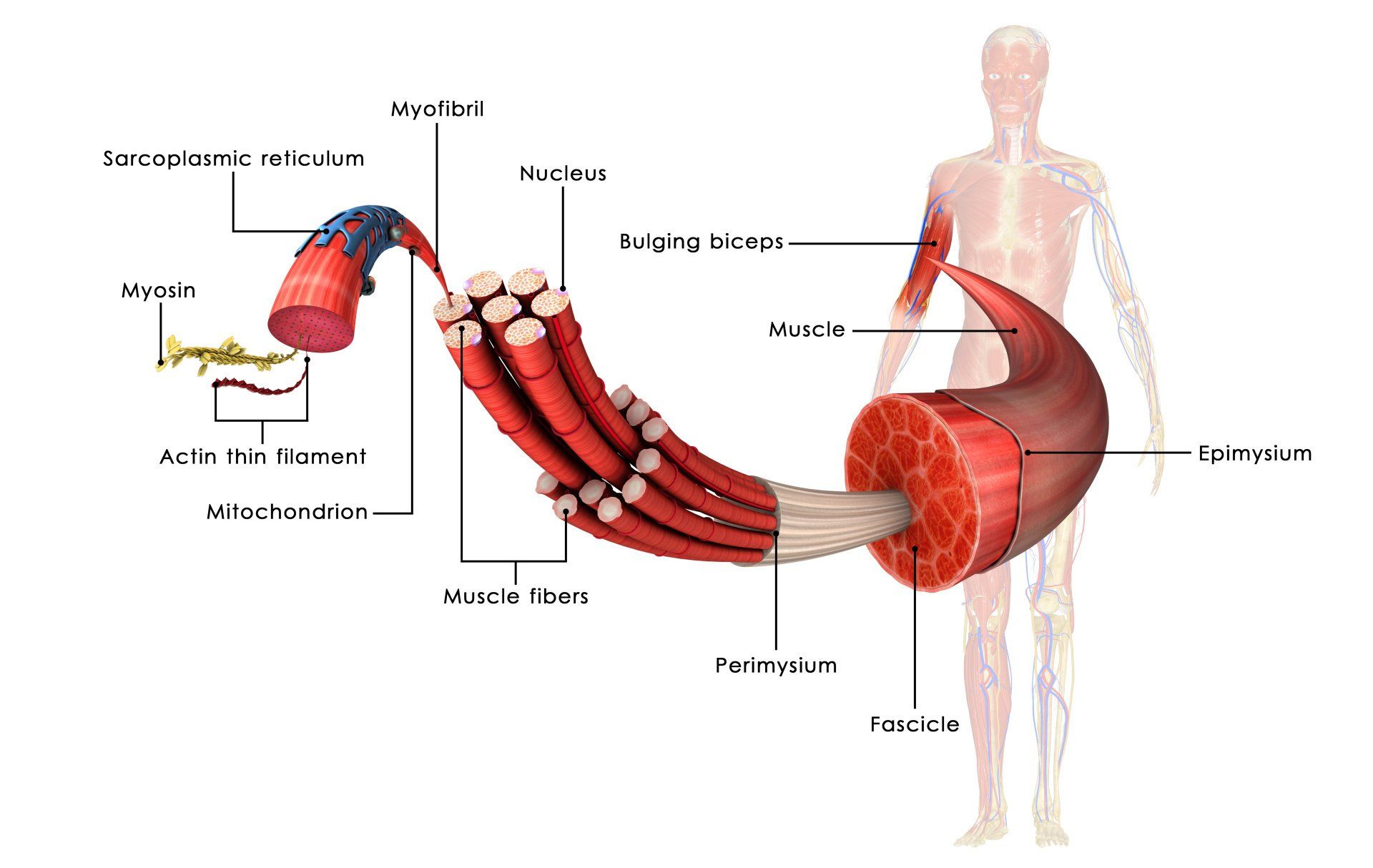
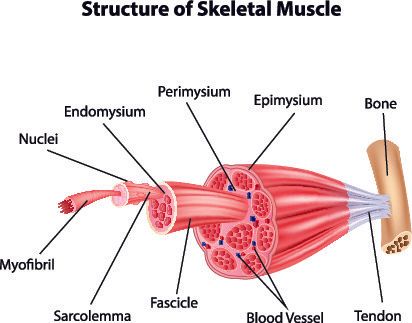
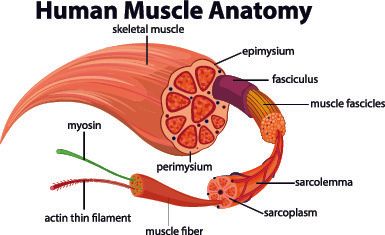
- Each muscle is enveloped in a connective tissue called epimysium
- Within the epimysium are numerous muscle fascicles which are enveloped by perimysium within which are numerous muscle fibres lined by endomysium
- Within the muscle fibre and numerous myofibrils and the individual functioning cell is called a sarcomere
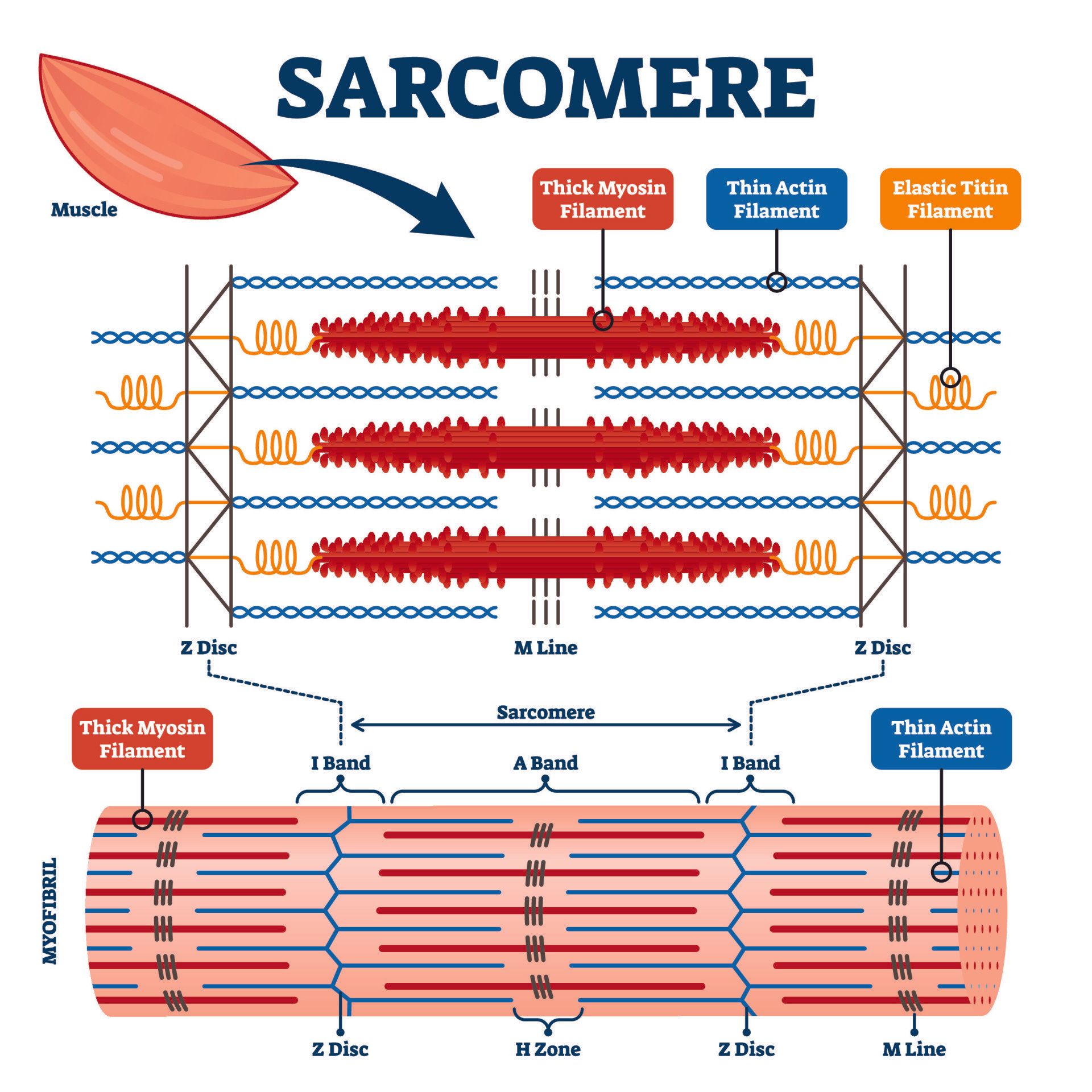
- Within a sarcomere are two filaments:
- Thick myosin filaments
- Thin actin filaments
- Muscle contraction occurs when an electrical impulse sent by a nerve to the muscle causes the release of calcium (from the sarcoplasmic reticulum)
- This release of calcium causes the actin filaments to attach to the myosin filaments and they pull on the myosin filament to cause shortening of the length of the sarcomere
- Energy (ATP) is required to detach the actin from the myosin and for the sarcomere to go back to its original resting length:
- That’s why when someone dies the muscles stay contracted as there is no new energy production to cause detachment of actin from myosin which is necessary for muscle relaxation
- This state is called rigor mortis and it is temporary for about 3 days
Some uniquely strong muscles
- Gluteus maximus is the largest muscle in the body:
- Helps maintain posture, standing from a sitting position and going upstairs
- The heart is the hardest working muscle in the body:
- The heart is about the size of your fist
- It beats about 115,000 times a day or 40 million times in a year and for an 80 year old that is 3.2 billion times!
- It pumps 6,000-7,500 litres a day
- Normal resting heart rate for an average adult male is 72 and for a female 80
- Athletes can have a resting heart rate of 40:
- They can achieve this by pumping more blood with each heart beat contraction (called stroke volume)
- The masseter (part of the jaw muscles) is the strongest muscle in the body compared to its weight:
- The strongest human bite strength produced 442kg for two seconds
- The external eye muscles work constantly to position the eye to help keep eyesight focused on a point whilst the body and head moves:
- In one hour, it can make 10,000 contractions
- Soleus is a muscle in the calf that lies deep to the more superficial and visible gastrocnemius muscle:
- It is thought to develop the greatest force of pull as it contracts against gravity to help us from falling over
Muscle fibre differences within skeletal muscle
- Skeletal muscle is made of individual muscle fibres
- They are broadly split into slow-twitch (type I) and fast twitch (type II) which can be further categorised into type IIa and IIb fibres
- The different types split the fibres into how they contract, what type of fuels they use and how they respond to physical training
- Type I (slow twitch):
- They react less slowly, produce less force but can do so over a longer period of time, and are more efficient at using oxygen to generate the fuel (called adenosine triphosphate or ATP) needed for the muscle contraction
- They are more fatigue resistant and are important for aerobic and endurance exercises e.g. marathon runners
- Type II (fast twitch):
- They are better at providing quick, short but more powerful bursts of strength or speed than slow twitch type I fibres
- They use an anaerobic metabolism which produces ATP in the absence of oxygen and are therefore quicker to fatigue
- Type IIa can be thought of as intermediate fast twitch fibres using both aerobic and anaerobic metabolism which explains their improved fatigue resistance compared to type IIb
- Type IIb fibres produce the greatest force and most rapidly compared to the other muscle fibres but fatigues quickest as it relies solely on anaerobic metabolism
The impact of training on muscle fibre types
- We all have all the types of muscle fibres
- The amount of force generated by a muscle is most dependent on its cross-sectional area than on the type of muscle fibre it has
- Duration and speed of contraction is most dependent on muscle fibre type
- Muscle fibre size increases with strength training
- Muscle fibre types are split equally in non-athletic individuals
- As we age there is not only loss of lean muscle mass but the fast twitch (especially type IIb) reduce in number whilst the proportion of type I increases
- With training the proportion of muscle fibres changes according to the exercises carried out
- Power athletes such as sprinters have predominantly type II muscle fibres (70-80%)
- Endurance athletes have predominantly type I muscle fibres (70-80%)
- Whilst training can increase the proportion of a a muscle fibre depending on the exercise, the elite athletes seem to have a genetic advantage in being able to achieve a higher percentage:
- However, without intense training to reach the maximum potential, genetics alone are not enough
Role of genetics on athletic performance
- Training, motivation, nutrition are key components in maximising performance of an athlete
- Genes are thought to contribute to 30-80% of the difference between individuals in factors that are key to athletic performance such as:
- Strength
- Muscle size
- Muscle fibre composition
- Lung capacity
- Anaerobic threshold which is when lactate builds up and the athlete tires out
- Cardiac output (ability of the heart to pump blood around the body in a given time)
- Ability of muscle to utilise oxygen and the energy molecule called ATP:
- The efficiency of this process is measured by VO2 max which shows the maximum amount of oxygen a person can use during intense exercise
- VO2 max is one of the key tests for the cardiovascular fitness of an athlete
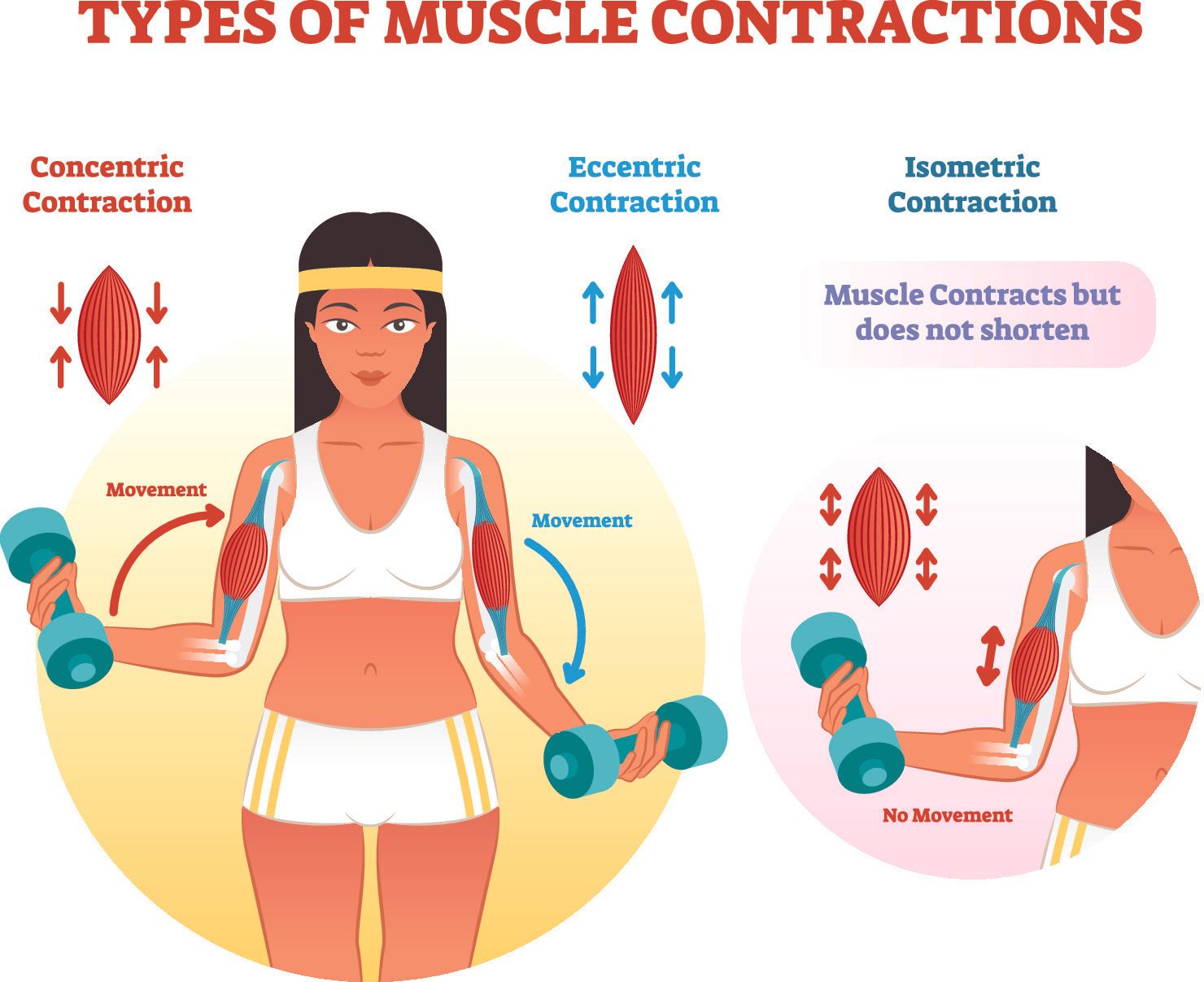
Types of muscle contraction
- Isometric:
- Muscle contracts with constant length e.g. holding a weight but not moving it or pushing against an immovable object
- Isotonic:
- Muscle contracts with constant tension e.g. lifting the same weight through a range of motion
- There are two types:
- Concentric:
- Muscle shortens during contraction e.g. biceps curl and bringing a weight from an outstretched hand position up to the shoulder by bending at the elbow
- This contraction is required to initiate a movement
- Eccentric:
- Muscle lengthens during contraction e.g. reverse biceps curl whereby the downward motion of the weight from the flexed elbow position to the arm straight, is performed slowly
- Eccentric training compared to concentric has been shown to cause greater muscle hypertrophy, muscle strength and flexibility as well as to help treat tendinopathies and makes tendons stronger
- Eccentric contractions occur to slow down and stop a movement
- Isokinetic:
- Muscles contract under constant speed
- This requires special equipment
- Plyometric:
- Rapid lengthening of a muscle followed by contraction
- Often involve the athlete to jump, hop or skip and exert maximum force over a short time interval e.g. box jumping
- Shown to improve strength, speed, power, speed of changing direction, balance, jumping, and bone density
- Have been shown to reduce risk of lower limb injuries in team sports
- However, activity should be supervised and athlete to be in good condition as the high sudden forces can cause injuries if done incorrectly by someone with insufficient strength and poor proprioception
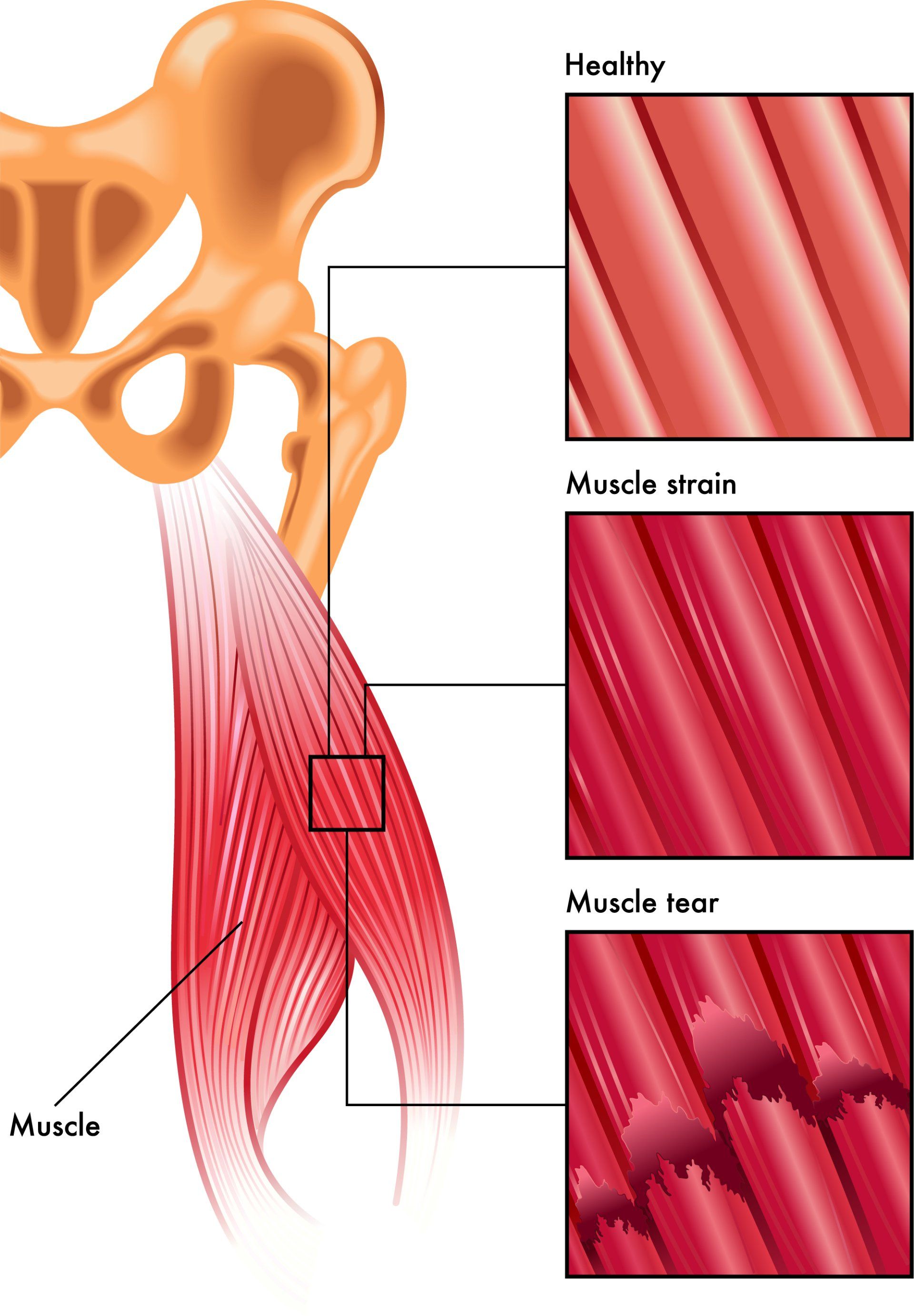
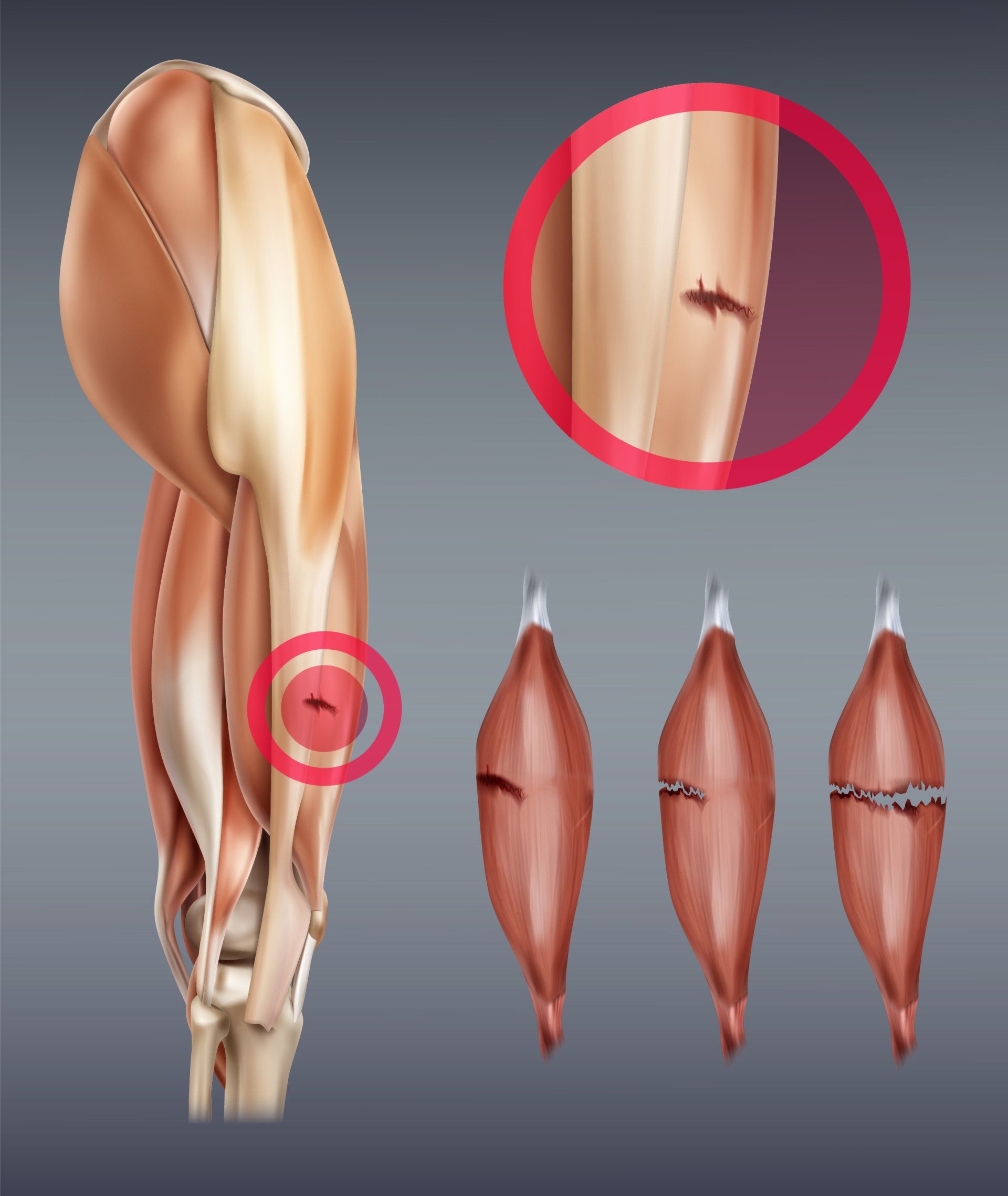
Muscle strain
- Muscle strain (commonly known as pulled muscle) occurs when a muscle is torn or overstretched
- They are most commonly due to fatigue or a heavy/rapid eccentric contraction
- Strains can occur in any muscle but are most common in the lower back, neck, hamstrings and shoulder
- Three muscle types are more prone to injuries:
- Muscles that cross over two joints:
- These are also called biarticular and as such influence the movement of two joints at the same time
- Examples of biarticular muscles around the knee are:
- Rectus femoris – primary action is to extend the knee, secondary is to flex the hip
- Gastrocnemius – primary action is to plantarflex the ankle (downward motion), secondary action is to flex the knee
- Hamstrings – composed of semitendinosus, semimembranosus, long head of biceps – primary action is to flex the knee and secondary is to extend the hip
- However functionally the biarticular muscles are important in controlling complex movement of the whole limb and they act primarily in an eccentric manner by helping decelerate the limb when it is swung forward preparing it for ground contact such as when we run and walk
- Movement of one joint will stretch the biarticular muscle which may then be required to contract forcefully at a very stretched position
- It is this eccentric contraction during a rapid movement such as sprinting and jumping that predisposes these muscles to injuries
- Muscles contracting eccentrically:
- Eccentric contractions are essential when we walk and run because they control movement of a limb by decelerating its movement
- The muscle is required to contract whilst at the same time lengthening (therefore placed under tension) at speed and if the muscle isn’t strong enough to overcome this tension then injury can occur
- Muscles with a higher percentage of type II fibres:
- Since type II fibres produce a large amount of force over a short period of time they are bound to be more susceptible to injuries
- These fibres predominate in muscles involved in sprinting which involves mostly eccentric contractions
- The most commonly injured muscles are those that have all three components such as: hamstrings, gastrocnemius, rectus femoris (the only part of the quadriceps muscle which is biarticular)
Symptoms of a muscle strain
- Sudden pain
- Bruising
- Swelling
- Stiffness with reduced range of movement
- Weakness
Treatment
- Rest:
- First few days should try and limit movement of the affected muscle
- After that movement needs to gradually start so as to prevent stiffness
- Ice:
- Ice should be applied immediately but should not be applied directly to skin
- Wrap a bag of peas in a pillow case or towel
- Apply for 20 minutes
- Compression:
- Applying pressure on the muscle with a suitably wrapped compression bandage will help reduce swelling and therefore pain
- This should not be applied though too tight so as not to adversely affect blood flow to the area as well as the distal part of the limb
- Elevation:
- Elevating the injured limb above the level of the heart will help reduce the swelling to that area
Ways to minimise risk of muscle strains
- Keeping muscles healthy, strong and flexible throughout life:
- This will also help keep tendons, ligaments and bones strong as well
- Warm up gradually before starting more strenuous activities:
- Try and focus on dynamic stretching before an exercise and static stretching afterwards (further information to this can be found in the lower limb injury prevention programme section)
- Build the intensity of your training programme gradually with rest periods in between and these rest periods need to be longer when the individual is less physically fit
- For the middle aged and elderly, it would be worth seeking a medical consultation prior to commencement of physical training
- Careful attention should be placed on correct technique at all times especially when lifting weights and carrying out high impact activities e.g. those involved in plyometrics and team sports
- If overweight try and lose weight first through lower impact activities (cycling, rowing, crosstrainer) and dieting prior to starting higher impact activities (jogging) in order to minimise the stresses to your lower limb joints
- Listen to your body:
- If something doesn’t feel right, stop and seek help
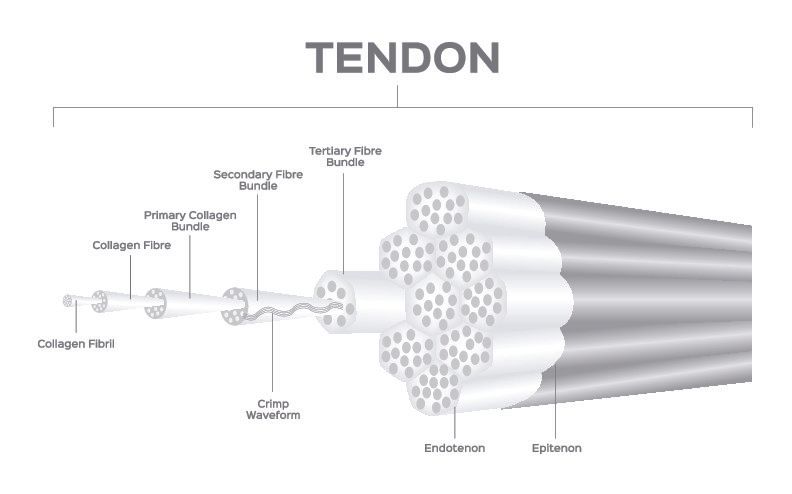
Tendon
- Tendons attach muscles to bone to enable the muscle to move the bone
- Each muscle has two tendinous attachments to a bone:
- The proximal tendon is called the origin
- The distal tendon is called the insertion
- Tendons have a very dense, organised and parallel array of collagen fibres
- Tendons are stronger but less elastic than ligament
Tendon injuries
- Tendon injuries most commonly occur at the musculotendinous junction:
- This is the area where the muscle turns into a tendon
- It is also the area of least blood supply which is why it is most commonly injured
Tendinopathy
- This is a chronic injury in a tendon resulting in a failed healing response
- The tendon is not ruptured but there is a breakdown in its collagen composition making it less strong but also very painful
- Tendinopathy is different from tendonitis:
- Tendonitis is inflammation of the tendon
- In tendinopathy there is no inflammatory reaction
- Unfortunately, all too commonly steroid injections are still used to treat tendinopathies despite research confirming that this is detrimental to its healing
- Treatment of tendinopathies is primarily:
- Activity modification by doing less of the activities that exacerbate the problem
- Assessment by a suitably qualified person to evaluate cause of the tendinopathy e.g. muscle imbalance around a joint
- Physiotherapy with exercises to address the muscle imbalance
- Loading the muscle of the tendon involved in ways to make it stronger:
- This will help change the collagen type III which is found in tendinopathies to collagen type I which is what it should have
Ligament
- A ligament is a fibrous connective tissue that connects bones to bones
- Whilst there are various types of ligaments, articular ones are the most common ones and they span across the joint surfaces connecting the bones above and below thus providing stability to the joint
- Ligaments are not as tough as tendons but they are more elastic
- Ligament injuries range from mild sprains with only a few fibres being torn to complete ruptures rendering the joint unstable
Ligament sprain
- Ligaments sprains are split into 3 grades
- Grade I sprain:
- Some stretched fibres but joint is still stable
- Mild to minimal swelling
- Grade II sprain:
- Moderate stretching of the ligament but overall is still in tact
- Examination shows increased laxity of the ligament but there is an end point
- Moderate swelling with perceived pain instability by patient on function
- Grade III sprain:
- Complete tear of the ligament
- Marked swelling and tenderness
- Gross instability with no firm end point when stressing the ligament on examination
Treatment
- Same initial principles of rest, ice, elevation and compression
- Grade I and II sprains are often treated with some type of splint or brace for 4-6 weeks
- Grade III sprains are more likely to need an operation to either repair or reconstruct the injured ligament
More relevant information can be found on:

Introduction Cubital Tunnel Syndrome occurs when the ulnar nerve is compressed within a tunnel on the inner (medial) side of the elbow just behind the bony prominence of the inner aspect of the elbow called the medial epicondyle Cubital Tunnel Syndrome is the second most common cause of peripheral nerve compression: The most common one being carpal tunnel syndrome (compression of the median nerve at the wrist) The ulnar nerve is one of the three main nerves of the upper limb: The other two nerves of the upper limb are the median nerve and the radial nerve The ulnar nerve travels from the neck past the elbow and wrist and into the hand: Along the way it travels past some narrow areas where it can be constricted and cause symptoms for the patient The most common site of ulnar nerve compression is in the cubital tunnel at the elbow The second most common site is in Guyon’s canal in the hand When someone accidentally hits the inner side of the elbow (often termed hitting the funny bone) they get a sharp tingling sensation on the inner side of the elbow and forearm: This occurs because the ulnar nerve was hit at the site of the cubital tunnel where the nerve is close to the skin surface and therefore easily injured from outside forces
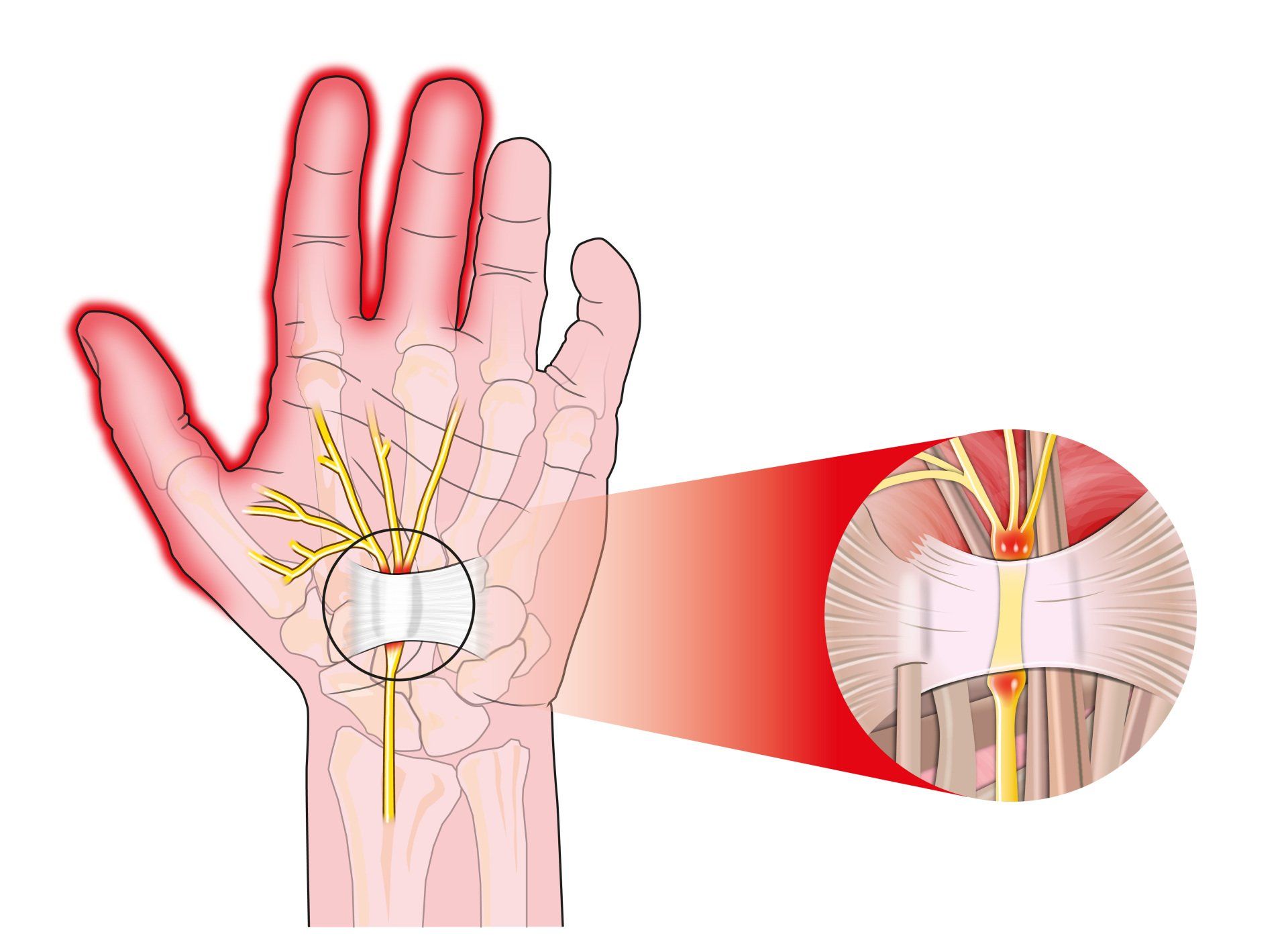
Introduction Carpal tunnel syndrome is a common condition that causes numbness, tingling and weakness in the hand specifically affecting the thumb, index and middle fingers: The little and ring fingers are not affected as they are supplied by another nerve called the ulnar nerve It is the commonest cause of peripheral nerve entrapment It is caused by compression of the median nerve as it passes from the forearm into the hand through a passage called carpal (i.e. wrist) tunnel The median nerve is one of three main nerves that supply the upper limb: The other two nerves are the ulnar nerve and the radial nerve
Introduction Tennis elbow (also known as lateral epicondylitis) is an overuse injury of the forearm tendons that originate over the lateral epicondyle of the humerus (bony prominence on the outside of the elbow) and act to bring the wrist backward away from the palm Whilst tennis players are particular prone to this condition it does not occur exclusively to them

Introduction This term is also known as repetitive motion or stress injury and occurs as a result of carrying out the same motion repeatedly over time causing injury to muscles and tendons It is associated with repetitive tasks, sustained or awkward position, forceful exertion, vibration or compressive forces It can affect almost any joint in the body Most commonly affected areas are hands, wrists, shoulders and neck It is thought to affect 5-10% of the general population but can be as high as 20-40% in specific working populations